| Membranoproliferative glomerulonephritis | |
|---|---|
| Other names | Mesangiocapillary glomerulonephritis[1] |
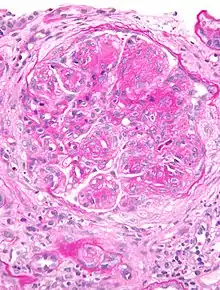 | |
| Micrograph of glomerulus in membranoproliferative glomerulonephritis with increased mesangial matrix and increased mesangial cellularity. Kidney biopsy. PAS stain. | |
| Specialty | Nephrology |
Membranoproliferative glomerulonephritis (MPGN) is a type of glomerulonephritis caused by deposits in the kidney glomerular mesangium and basement membrane (GBM) thickening,[2] activating the complement system and damaging the glomeruli.
MPGN accounts for approximately 4% of primary renal causes of nephrotic syndrome in children and 7% in adults.[3]
It should not be confused with membranous glomerulonephritis, a condition in which the basement membrane is thickened, but the mesangium is not.
Type
There are three types of MPGN, but this classification is becoming obsolete as the causes of this pattern are becoming understood.
Type I
Type I, the most common by far, is caused by immune complexes depositing in the kidney. It is characterised by subendothelial and mesangial immune deposits.
It is believed to be associated with the classical complement pathway.[4]
Type II – Dense deposit disease
Type II is today more commonly known as dense deposit disease (DDD).[5] Most cases of dense deposit disease do not show a membranoproliferative pattern.[6] It forms a continuum with C3 glomerulonephritis; together they make up the two major subgroups of C3 glomerulopathy.[7]
Most cases are associated with the dysregulation of the alternative complement pathway.[8][9]
DDD is associated with deposition of complement C3 within the glomeruli with little or no staining for immunoglobulin. The presence of C3 without significant immunoglobulin suggested to early investigators that DDD was due to abnormal activation of the complement alternative pathway (AP). There is now strong evidence that DDD is caused by uncontrolled AP activation.[10]
Spontaneous remissions of MPGN II are rare; approximately half of those affected with MPGN II will progress to end stage renal disease within ten years.[11]
In many cases, people with MPGN II can develop drusen caused by deposits within Bruch's membrane beneath the retinal pigment epithelium of the eye. Over time, vision can deteriorate, and subretinal neovascular membranes, macular detachment, and central serous retinopathy can develop.[12]
Type III
Type III is very rare, it is characterized by a mixture of subepithelial and subendothelial immune and/or complement deposits. These deposits elicit an immune response, causing damage to cells and structures within their vicinity. Has similar pathological findings of Type I disease.[13]
A candidate gene has been identified on chromosome 1.[14]
Complement component 3 is seen under immunofluorescence.[15] it is associated with complement receptor 6 deficiency.
Pathology
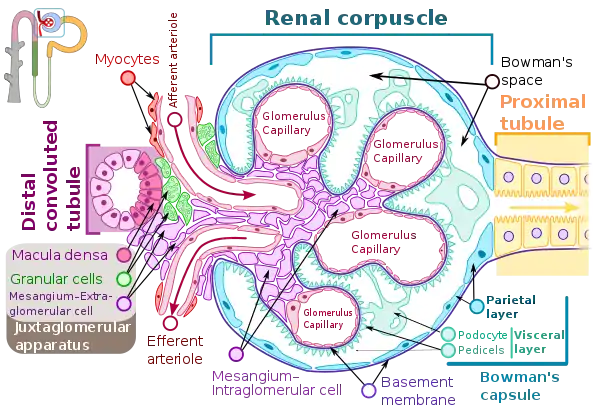
Membranoproliferative glomerulonephritis involves deposits at the intraglomerular mesangium.
It is also the main hepatitis C associated nephropathy.
It also is related to a number of autoimmune diseases, prominently systemic lupus erythematosus (SLE), Class IV. Also found with Sjögren syndrome, rheumatoid arthritis, inherited complement deficiencies (esp C3 deficiency), scleroderma, Celiac disease.[16]
The histomorphologic differential diagnosis includes transplant glomerulopathy and thrombotic microangiopathies.
Diagnosis
The GBM is rebuilt on top of the deposits, causing a "tram tracking" appearance under the microscope.[17] Mesangial cellularity is increased.[18]
Treatment
Primary MPGN is treated with steroids, plasma exchange and other immunosuppressive drugs. Secondary MPGN is treated by treating the associated infection, autoimmune disease or neoplasms. Pegylated interferon and ribavirin are useful in reducing viral load. [19]
See also
References
- ↑ Colville D, Guymer R, Sinclair RA, Savige J (August 2003). "Visual impairment caused by retinal abnormalities in mesangiocapillary (membranoproliferative) glomerulonephritis type II ("dense deposit disease")". Am. J. Kidney Dis. 42 (2): E2–5. doi:10.1016/S0272-6386(03)00665-6. PMID 12900843.
- ↑ "membranoproliferative glomerulonephritis" at Dorland's Medical Dictionary
- ↑ Habib R, Gubler MC, Loirat C, Mäiz HB, Levy M (1975). "Dense deposit disease: a variant of membranoproliferative glomerulonephritis". Kidney Int. 7 (4): 204–15. doi:10.1038/ki.1975.32. PMID 1095806.
- ↑ West CD, McAdams AJ (March 1998). "Glomerular paramesangial deposits: association with hypocomplementemia in membranoproliferative glomerulonephritis types I and III". Am. J. Kidney Dis. 31 (3): 427–34. doi:10.1053/ajkd.1998.v31.pm9506679. PMID 9506679.
- ↑ Niepolski, Leszek; Czekała, Anna; Seget-Dubaniewicz, Monika; Frydrychowicz, Magdalena; Talarska-Markiewicz, Patrycja; Kowalska, Angelika; Szmelter, Jagoda; Salwa-Żurawska, Wiesława; Sirek, Tomasz; Sobański, Dawid; Grabarek, Beniamin Oskar; Żurawski, Jakub (2023-04-05). "Diagnostic Problems in C3 Glomerulopathy". Biomedicines. 11 (4): 1101. doi:10.3390/biomedicines11041101. ISSN 2227-9059. PMC 10135645. PMID 37189718.
- ↑ Patrick D Walker; Franco Ferrario; Kensuke Joh; Stephen M Bonsib (2007). "Dense deposit disease is not a membranoproliferative glomerulonephritis". Modern Pathology. 20 (6): 605–616. doi:10.1038/modpathol.3800773. PMID 17396142.
- ↑ Smith, Richard J.H.; Appel, Gerald B.; Blom, Anna M.; Cook, H. Terence; D’Agati, Vivette D.; Fakhouri, Fadi; Fremeaux-Bacchi, Véronique; Józsi, Mihály; Kavanagh, David; Lambris, John D.; Noris, Marina; Pickering, Matthew C.; Remuzzi, Giuseppe; de Córdoba, Santiago Rodriguez; Sethi, Sanjeev (March 2019). "C3 glomerulopathy — understanding a rare complement-driven renal disease". Nature Reviews. Nephrology. 15 (3): 129–143. doi:10.1038/s41581-018-0107-2. ISSN 1759-5061. PMC 6876298. PMID 30692664.
- ↑ Rose KL, Paixao-Cavalcante D, Fish J, et al. (February 2008). "Factor I is required for the development of membranoproliferative glomerulonephritis in factor H-deficient mice". J. Clin. Invest. 118 (2): 608–18. doi:10.1172/JCI32525. PMC 2200299. PMID 18202746.
- ↑ Licht C, Schlötzer-Schrehardt U, Kirschfink M, Zipfel PF, Hoppe B (January 2007). "MPGN II--genetically determined by defective complement regulation?". Pediatr. Nephrol. 22 (1): 2–9. doi:10.1007/s00467-006-0299-8. PMID 17024390. S2CID 14776253.
- ↑ (reviewed in Appel et al., 2005; Smith et al., 2007). Smith, R. J. ., Harris, C. L., & Pickering, M. C. (2011). Dense Deposit Disease. Molecular Immunology, 48(14), 1604–1610. http://doi.org/10.1016/j.molimm.2011.04.005/
- ↑ Swainson CP, Robson JS, Thomson D, MacDonald MK (1983). "Mesangiocapillary glomerulonephritis: a long-term study of 40 cases". J. Pathol. 141 (4): 449–68. doi:10.1002/path.1711410404. PMID 6363655. S2CID 25434508.
- ↑ Colville D, Guymer R, Sinclair RA, Savige J (2003). "Visual impairment caused by retinal abnormalities in mesangiocapillary (membranoproliferative) glomerulonephritis type II ("dense deposit disease")". Am. J. Kidney Dis. 42 (2): E2–5. doi:10.1016/S0272-6386(03)00665-6. PMID 12900843.
- ↑ Pickering, M. C., D’Agati, V. D., Nester, C. M., Smith, R. J., Haas, M., Appel, G. B., … Cook, H. T. (2013). C3 glomerulopathy: consensus report. Kidney International, 84(6), 1079–1089. http://doi.org/10.1038/ki.2013.377
- ↑ Neary JJ, Conlon PJ, Croke D, et al. (August 2002). "Linkage of a gene causing familial membranoproliferative glomerulonephritis type III to chromosome 1". J. Am. Soc. Nephrol. 13 (8): 2052–7. doi:10.1097/01.ASN.0000022006.49966.F8. PMID 12138136.
- ↑ Neary J, Dorman A, Campbell E, Keogan M, Conlon P (July 2002). "Familial membranoproliferative glomerulonephritis type III". Am. J. Kidney Dis. 40 (1): e1.1–e1.6. doi:10.1053/ajkd.2002.33932. PMID 12087587.
- ↑ "UpToDate".
- ↑ "Membranoproliferative_glomerulonephritis_type_I of the Kidney". Archived from the original on 2006-09-10. Retrieved 2008-11-25.
- ↑ "Renal Pathology". Retrieved 2008-11-25.
- ↑ Harrison's principles of internal medicine (19th ed.). New York, NY: McGraw-Hill Companies, Inc. 2015. p. 1841. ISBN 978-0-07-180216-1.
External links
- Glomerulonephritis, Membranoproliferative Types I, II, III at eMedicine
- Corchado, Johnny Cruz, Smith, Richard JH (July 2007). "Dense Deposit Disease/Membranoproliferative Glomerulonephritis Type II". In Pagon RA, Bird TD, Dolan CR, et al. (eds.). GeneReviews. Seattle WA: University of Washington. PMID 20301598.
- Membranoproliferative_GN at Nephropathology tutorial
- MP GN Pathophysiology discusses the nephritic auto-antibodies/factors