| Bovine papillomaviruses | |
|---|---|
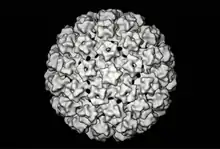 | |
| Bovine papillomavirus (3D reconstruction) | |
| Scientific classification | |
| (unranked): | Virus |
| Realm: | Monodnaviria |
| Kingdom: | Shotokuvirae |
| Phylum: | Cossaviricota |
| Class: | Papovaviricetes |
| Order: | Zurhausenvirales |
| Family: | Papillomaviridae |
| Subfamily: | Firstpapillomavirinae |
| Groups included | |
| |
Bovine papillomaviruses (BPV) are a paraphyletic group of DNA viruses of the subfamily Firstpapillomavirinae of Papillomaviridae that are common in cattle. All BPVs have a circular double-stranded DNA genome. Infection causes warts (papillomas and fibropapillomas) of the skin and alimentary tract, and more rarely cancers of the alimentary tract and urinary bladder. They are also thought to cause the skin tumour equine sarcoid in horses and donkeys.
BPVs have been used as a model for studying papillomavirus molecular biology and for dissecting the mechanisms by which this group of viruses cause cancer.
Structure and genetic organisation
Like other papillomaviruses, BPVs are small non-enveloped viruses with an icosahedral capsid around 50–60 nm in diameter.[2][3] The capsid is formed of the L1 and L2 structural proteins, with the L1 C-terminus exposed.[2][4]
All BPVs have a circular double-stranded DNA genome of 7.3–8.0 kb. The genetic organisation of those BPVs which have been sequenced is broadly similar to other papillomaviruses. The open reading frames (ORFs) are all located on one strand, and are divided into early and late regions. The early region encodes nonstructural proteins E1 to E7. There are three viral oncoproteins, E5, E6 and E7; BPVs of the Xipapillomavirus group lack E6. The late region encodes structural proteins L1 and L2. There is also a non-coding long control region (LCR).[2]
Types
Six types of BPV have been characterised, BPV-1 to BPV-6, which are divided into three broad subgroups.
- Deltapapillomavirus or fibropapillomaviruses (formerly known as subgroup A), including types 1 and 2, have a genome of around 7.9 kb. Similar papillomaviruses of ungulates (e.g. deer papillomavirus, European elk papillomavirus, ovine papillomavirus 1,2) are also found in this group. Like all members of the papillomavirus class, these viruses infect only keratinocytes (epithelial cells); however, unlike other papillomaviruses, they cause proliferation of both keratinocytes and fibroblasts, causing benign fibropapillomas involving both the epithelium and the underlying dermis. The specificity of the types differs:
- BPV-1 infects paragenital areas, including penis, teats and udders
- BPV-2 infects skin, alimentary canal and urinary bladder
- Xipapillomavirus or epitheliotropic BPVs (formerly known as subgroup B), including types 3, 4 and 6, have a smaller genome of around 7.3 kb and are unique among papillomaviruses in lacking the E6 oncoprotein.[3] They infect keratinocytes (epithelial cells), causing pure papillomas involving only the epithelium. The specificity of the types differs:
- BPV-3 infects skin
- BPV-4 infects the upper alimentary tract
- BPV-6 infects teats and udders
- Epsilonpapillomavirus has the single member BPV-5, with features intermediate between the other two groups. BPV-5 infects teats and udders, and can cause both pure papillomas and fibropapillomas.
A further thirteen putative BPVs have recently been identified; the novel viruses have yet to be assigned to subgroups.[5]
Pathology

BPV is highly prevalent, with around 50% of cattle being estimated to bear lesions in the UK.[6] Cutaneous warts are most common in younger animals (under 2 years) and usually spontaneously regress due to the animal's immune response without significant scarring. The duration of infection is very variable (from one month to over a year) and recurrence is possible.[7]
Warts caused by the Xipapillomavirus group have a cauliflower-like appearance and can attain the size of a fist; most common on the head, neck and shoulders, they may also occur in other locations.[7] Cutaneous fibropapillomas caused by Deltapapillomavirus group have a nodular appearance.[7] Although unsightly, most skin warts rarely cause problems except in show animals. However, large warts may bleed, potentially leading to secondary infections, and florid warts of the teat can cause mastitis and interfere with suckling and milking.[3] Fibropapillomas can be troublesome when present in the genital area, causing pain and sometimes loss of reproductive functions as well as interfering with calving.[3][7] Chronically immunosuppressed animals may develop extensive papillomatosis in the upper gastrointestinal tract, which can cause difficulties with eating and breathing.[3]

Warts contain large amounts of infectious virus which is relatively stable. Transmission between animals is common via, for example, fence posts or halters. Warts on the teats of lactating cows are readily transmitted to calves via abrasions. Contaminated tattooing or tagging equipment is another common source of infection.
Association with cancer
Cattle
BPV-4 causes squamous cell carcinomas of the alimentary tract, and BPV-1/2 causes carcinomas and haemangioendotheliomas of the urinary bladder, in both cases in animals that have fed on bracken (Pteridium aquilinum).[3] Such cancers are common in locations where grazing land is infested with bracken, such as the western Scottish Highlands, southern Italy and the Nasampolai Valley in Kenya.[3] Bracken contains several immunosuppressants and mutagens, including quercetin and ptaquiloside. Consumption of large quantities by cattle leads to an acute poisoning syndrome[8] with symptoms of bone marrow depletion, while at lower levels of long-term consumption it acts as a cancer cofactor.[3][9] Carcinogenesis is a multistep process; tumours also contain activated Ras, as well as mutation or downregulation of the tumour suppressor genes p53 in alimentary tract cancers and fragile histidine tetrads (FHIT) in urinary bladder cancers.[3] Viral particles are not produced in either alimentary tract or urinary bladder tumours.[3]

These bracken-associated tumours might form a model for some types of human oesophageal cancer. Human papillomavirus DNA has been detected in around 18% of squamous cell carcinomas of the oesophagus,[10] and there is an association between exposure to or consumption of bracken (which is used as a foodstuff and herbal remedy in South America, China, Japan, Korea and other countries) and risk of developing oesophageal cancer.[3]
Other mammals
BPV-1 and BPV-2 can also induce sarcomas and fibrosarcomas in other mammals, including equids (equine sarcoid)[11] and, experimentally, rabbits, hamsters and mice[12][13] (and reviewed in[2]). Viral particles are not produced during infection of other species and, unlike in tumours associated with human papillomavirus, the viral DNA is not integrated into the host genome.[11]
Equine sarcoid, a naturally occurring skin tumour affecting horses, donkeys and mules, is associated with strains of BPV-1/2 which may be equine specific.[11] The lesions can occur anywhere on the body, often multiply, with the limbs, thorax–abdomen, head and paragenital areas being particularly commonly affected.[11][14] The method of transmission is currently unclear; the involvement of face flies (Musca autumnalis) has been suggested, and transmission via contaminated tack is likely.[11] The disease forms the only known example of natural cross-species infection by a papillomavirus. The involvement of BPV leads to hope that vaccination or antiviral therapy might be possible in the future for this common tumour.
Treatment, prophylaxis and prevention
Treatment is not usually required, as most warts eventually regress spontaneously. Surgical removal is possible but may lead to recurrence.[7] Disinfection with formaldehyde of stalls, fence posts and other environmental virus reservoirs can prevent transmission.[7]
Vaccination
Vaccines against BPV types 1, 2 and 4 have been developed by M. Saveria Campo and others.[3][6]
- Prophylactic vaccination (i.e., vaccination of wart-free animals to prevent infection) with whole virus (e.g. formalin-killed wart tissue suspension), virus-like particles (L1 or L1+L2), L1 protein or (for BPV-4) L2 protein confers long-lasting protection against challenge with the same BPV type, but is generally ineffective against existing warts. Protection appears to be mediated via type-specific neutralising antibodies.[3] Vaccination of calves as early as 4–6 weeks might be necessary to prevent infection.[7]
- Therapeutic vaccination (i.e., vaccination of animals with existing warts) with BPV-4 E7 or BPV-2 L2 induces early regression of warts. Wart rejection involves a cell-mediated immune response, with infiltration of the site by large numbers of lymphocytes and macrophages.[3]
These vaccine systems have served as models for the successful development of prophylactic vaccines against the human papillomavirus types associated with cervical and anal cancers.[15] Both Gardasil (a quadrivalent prophylactic HPV vaccine licensed in 2006) and Cervarix (a bivalent prophylactic vaccine license in the EU in 2007 and USA in 2009) contain virus-like particles assembled from L1 protein, an approach successful against BPV, and both vaccines induce sustained immunity.[16][17] Various therapeutic HPV vaccines based on E6, E7 and L2 are currently in early-stage clinical trials.[18]
References
- 1 2 3 "ICTV Taxonomy history: Bovine papillomavirus 1". International Committee on Taxonomy of Viruses (ICTV). Retrieved 17 January 2019.
- 1 2 3 4 Shah KV, Howley PM (1996). "Papillomaviruses". In Fields BN, Knipe DM, Howley PM, et al. (eds.). Fields Virology (3rd ed.). Lippincott-Raven.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Campo, MS (2006). "Bovine papillomavirus: old system, new lessons?". In Campo, MS (ed.). Papillomavirus Research: From Natural History to Vaccine and Beyond. Caister Academic. ISBN 978-1-904455-04-2.
- ↑ Modis Y, Trus BL, Harrison SC (2002). "Atomic model of the papillomavirus capsid". EMBO J. 21 (18): 4754–62. doi:10.1093/emboj/cdf494. PMC 126290. PMID 12234916.
- ↑ Ogawa T, Tomita Y, Okada M, Shinozaki K, Kubonoya H, Kaiho I, Shirasawa H (2004). "Broad-spectrum detection of papillomaviruses in bovine teat papillomas and healthy teat skin". J. Gen. Virol. 85 (Pt 8): 2191–7. doi:10.1099/vir.0.80086-0. PMID 15269358.
- 1 2 Campo, MS (1995). "Infection by bovine papillomavirus and prospects for vaccination". Trends Microbiol. 3 (3): 92–7. doi:10.1016/s0966-842x(00)88889-7. PMID 7773594.
- 1 2 3 4 5 6 7 "Veterinary Manual".
- ↑ "Veterinary Manual".
- ↑ Jarrett WF, McNeil PE, Grimshaw WT, Selman IE, McIntyre WI (1978). "High incidence area of cattle cancer with a possible interaction between an environmental carcinogen and a papilloma virus". Nature. 274 (5668): 215–7. Bibcode:1978Natur.274..215M. doi:10.1038/274215a0. PMID 210386. S2CID 4172497.
- ↑ Syrjänen KJ (2002). "HPV infections and oesophageal cancer". J. Clin. Pathol. 55 (10): 721–8. doi:10.1136/jcp.55.10.721. PMC 1769774. PMID 12354793.
- 1 2 3 4 5 Chambers G, Ellsmore VA, O'Brien PM, Reid SW, Love S, Campo MS, Nasir L (2003). "Association of bovine papillomavirus with the equine sarcoid". J. Gen. Virol. 84 (Pt 5): 1055–62. doi:10.1099/vir.0.18947-0. PMID 12692268.
- ↑ Boiron M, Levy JP, Thomas M, Friedmann JC, Bernard J (1964). "Some properties of Bovine papilloma virus". Nature. 201 (4917): 423–4. Bibcode:1964Natur.201..423B. doi:10.1038/201423a0. PMID 14110027. S2CID 4276918.
- ↑ Robl MG, Olson C (1968). "Oncogenic action of bovine papilloma virus in hamsters". Cancer Res. 28 (8): 1596–604. PMID 4300248.
- ↑ "Veterinary Manual".
- ↑ "HPV Symptoms, Treatment, Vaccine, HPV in Men and Women". www.std-gov.org. 2015-05-09.
- ↑ Markowitz LE, Dunne EF, Saraiya M, Lawson HW, Chesson H, Unger ER (2007). "Quadrivalent Human Papillomavirus Vaccine: Recommendations of the Advisory Committee on Immunization Practices (ACIP)". MMWR Recomm Rep. 56 (RR-2): 1–24. PMID 17380109.
- ↑ Harper DM, Franco EL, Wheeler CM, Moscicki AB, Romanowski B, Roteli-Martins CM, Jenkins D, Schuind A, Costa Clemens SA, Dubin G (2006). "Sustained efficacy up to 4.5 years of a bivalent L1 virus-like particle vaccine against human papillomavirus types 16 and 18: follow-up from a randomised control trial". Lancet. 367 (9518): 1247–55. doi:10.1016/S0140-6736(06)68439-0. PMID 16631880. S2CID 18685310.
- ↑ Davidson EJ, Faulkner RL, Sehr P, Pawlita M, Smyth LJ, Burt DJ, Tomlinson AE, Hickling J, Kitchener HC, Stern PL (2004). "Effect of TA-CIN (HPV 16 L2E6E7) booster immunisation in vulval intraepithelial neoplasia patients previously vaccinated with TA-HPV (vaccinia virus encoding HPV 16/18 E6E7)". Vaccine. 22 (21–22): 2722–9. doi:10.1016/j.vaccine.2004.01.049. PMID 15246603.