The Cobb angle is a measurement of bending disorders of the vertebral column such as scoliosis and traumatic deformities.
Definition and method
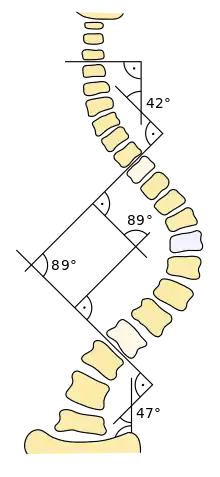
It is defined as the greatest angle at a particular region of the vertebral column, when measured from the superior endplate of a superior vertebra to the inferior endplate of an inferior vertebra.[1] However, the endplates are generally parallel for each vertebra, so not all sources include usage of a superior versus inferior endplate in the definition.[2]
Unless otherwise specified it is generally presumed to refer to angles in the coronal plane, such as projectional radiography in posteroanterior view. In contrast, a sagittal Cobb angle is one measured in the sagittal plane such as on lateral radiographs.[3]
Cobb angles are preferably measured while standing, since laying down decreases Cobb angles by around 7–10°.[4]
Uses
It is a common measurement of scoliosis.
The Cobb angle is also the preferred method of measuring post-traumatic kyphosis in a recent meta-analysis of traumatic spine fracture classifications.[5]
Severity
| Severity | Cobb angle |
|---|---|
| Not scoliosis | <10°[6] |
| Mild scoliosis | 10–30° |
| Moderate scoliosis | 30–45°[7] |
| Severe scoliosis | >45°[7] |
Those with Cobb angle of more than 60° usually have respiratory complications.[7]
Scoliosis cases with Cobb angles between 40 and 50 degrees at skeletal maturity progress at an average of 10 to 15 degrees during a normal lifetime. Cobb angles of more than 50 degrees at skeletal maturity progress at about 1 to 2 degrees per year.[8]
History
The Cobb angle is named after the American orthopedic surgeon John Robert Cobb (1903–1967). It was originally used to measure coronal plane deformity on radiographs with antero-posterior projection for the classification of scoliosis.[9] It has subsequently been adapted to classify sagittal plane deformity, especially in the setting of traumatic thoracolumbar spine fractures.
References
- ↑ Brian D. Coley (2013). Caffey's Pediatric Diagnostic Imaging (12 ed.). Elsevier Health Sciences. p. 1429. ISBN 978-1455753604.
- ↑ Fred F. Ferri (2017). Ferri's Clinical Advisor 2018 E-Book. Elsevier Health Sciences. p. 1150. ISBN 978-0323529570.
- ↑ Schmitz, A.; Jaeger, U.; Koenig, R.; Kandyba, J.; Gieske, J.; Schmitt, O. (2001). "Sagittale Cobb-Winkel-Messungen bei Skoliose mittels MR-Ganzwirbelsäulenaufnahme". Zeitschrift für Orthopädie und ihre Grenzgebiete. 139 (4): 304–07. doi:10.1055/s-2001-16915. ISSN 0044-3220. PMID 11558047. S2CID 260354772.
- ↑ Keenan, Bethany E; Izatt, Maree T; Askin, Geoffrey N; Labrom, Robert D; Pearcy, Mark J; Adam, Clayton J (2014). "Supine to standing Cobb angle change in idiopathic scoliosis: the effect of endplate pre-selection". Scoliosis. 9 (1): 16. doi:10.1186/1748-7161-9-16. ISSN 1748-7161. PMC 4193912. PMID 25342959.
- ↑ Keynan, Ory; Fisher, CG; Vaccaro, A; Fehlings, MG; Oner, FC; Dietz, J; Kwon, B; Rampersaud, R; Bono, C; France, J; Dvorak, M (Mar 1, 2006). "Radiographic measurement parameters in thoracolumbar fractures: a systematic review and consensus statement of the spine trauma study group" (PDF). Spine. 31 (5): E156–65. doi:10.1097/01.brs.0000201261.94907.0d. PMID 16508540. S2CID 39799085. Archived from the original (PDF) on 9 October 2013. Retrieved 15 December 2012.
- ↑ Page 89 in: Dr. Kevin Lau. The Complete Scoliosis Surgery Handbook for Patients: An In-Depth and Unbiased Look Into What to Expect Before and During Scoliosis Surgery. Health In Your Hands. ISBN 978-9810785925.
- 1 2 3 Page 460 in: Konrad E. Bloch, Thomas Brack, Anita K. Simonds (2015). ERS Handbook: Self-Assessment in Respiratory Medicine. European Respiratory Society. ISBN 978-1849840781.
{{cite book}}: CS1 maint: multiple names: authors list (link) - ↑ Greiner KA (2002). "Adolescent idiopathic scoliosis: radiologic decision-making". Am Fam Physician. 65 (9): 1817–22. PMID 12018804.
- ↑ Cobb JR. Outline for the study of scoliosis. The American Academy of Orthopedic Surgeons Instructional Course Lectures. Vol. 5. Ann Arbor, MI: Edwards; 1948.