| Melanosis coli | |
|---|---|
| Other names | Pseudomelanosis coli, |
 | |
| Melanosis coli identified on colonoscopy as a brownish moiré pattern on the wall of the colon. | |
Melanosis coli, also pseudomelanosis coli, is a disorder of pigmentation of the wall of the colon, often identified at the time of colonoscopy. It is benign and may have no significant correlation with disease. The brown pigment is lipofuscin in macrophages, not melanin. It is most commonly associated with the use of certain laxatives.
Cause
The most common cause of melanosis coli is the extended use of laxatives, and commonly anthraquinone containing laxatives such as senna, aloe vera, and other plant glycosides.[1] The anthranoid laxatives pass through the gastrointestinal tract unabsorbed until they reach the large intestine, where they are changed into their active forms. The resulting active compounds cause damage to the cells in the lining of the intestine and leads to apoptosis (a form of cell death). The damaged (apoptotic) cells appear as darkly pigmented bodies that may be taken up by scavenger cells known as macrophages. When enough cells have been damaged, the characteristic pigmentation of the bowel wall develops. The condition can develop after just a few months of laxative use.[2]
However, other causes are identified, including an increase in colonic epithelial apoptosis.[3] Endoscopically, the mucosa may show a brownish discoloration in a moiré pattern.
Histologic appearance
On biopsy, melanosis coli shows characteristic pigment-laden macrophages within the mucosa on PAS staining.[4]
The histologic differential diagnosis of mucosal pigmentation is: lipofuscin (melanosis coli), hemosiderin-laden macrophages, and melanin (rare).
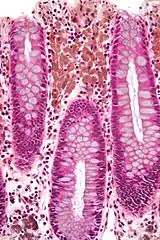
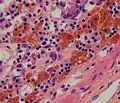 Micrograph showing melanosis coli, which appears as brown pigmentation in the macrophages in the lamina propria.
Micrograph showing melanosis coli, which appears as brown pigmentation in the macrophages in the lamina propria. Micrograph of melanosis coli. H&E stain.
Micrograph of melanosis coli. H&E stain. Micrograph of melanosis coli. H&E stain.
Micrograph of melanosis coli. H&E stain.
Prognosis
No adverse effects or consequences of melanosis coli have been identified.[4]
Relation to true melanoses
The condition is unrelated to true melanoses, such as Peutz–Jeghers syndrome and smoker's melanosis.[5]
Peutz–Jeghers syndrome causes pigmentation of the skin and mucous surfaces with melanin, and polyps in the digestive tract.
Non-colonic pseudomelanoses
Pseudomelanoses of other parts of the gastrointestinal tract have also been reported, and are of unclear relevance.[6]
Patients with colostomies can have melanosis involving the stoma, which is also of no significance.[7]
References
- ↑ Müller-Lissner, SA. (Oct 1993). "Adverse effects of laxatives: fact and fiction". Pharmacology. 47 (Suppl 1): 138–45. doi:10.1159/000139853. PMID 8234421.
- ↑ "What is Melanosis Coli? Symptoms, Causes & Treatment".
- ↑ Byers, R.J.; Marsh, P.; Parkinson, D.; Haboubi, N.Y (October 2003). "Melanosis coli is associated with an increase in colonic epithelial apoptosis and not with laxative use". Histopathology. 30 (2): 160–164. doi:10.1046/j.1365-2559.1997.d01-574.x. PMID 9067741. S2CID 3175917.
- 1 2 Wittoesch, JH.; Jackman, RJ.; McDonald, JR. (1958). "Melanosis coli: general review and a study of 887 cases". Dis Colon Rectum. 1 (3): 172–80. doi:10.1007/bf02616828. PMID 13537819. S2CID 46183745.
- ↑ Vellappally, S.; Fiala, Z.; Smejkalová, J.; Jacob, V.; Somanathan, R. (2007). "Smoking related systemic and oral diseases". Acta Medica. 50 (3): 161–6. doi:10.14712/18059694.2017.76. PMID 18254267.
- ↑ Ghadially, FN.; Walley, VM. (Sep 1994). "Melanoses of the gastrointestinal tract". Histopathology. 25 (3): 197–207. doi:10.1111/j.1365-2559.1994.tb01319.x. PMID 7821887. S2CID 22088870.
- ↑ Fleischer, I.; Bryant, D. (May 1995). "Melanosis coli or mucosa ischemia? A case report". Ostomy Wound Manage. 41 (4): 44, 46–7. PMID 7598783.