| Aspirin-exacerbated respiratory disease | |
|---|---|
| Other names | Aspirin-induced asthma, Samter's triad, Samter's syndrome, nonsteroidal anti-inflammatory drug (NSAID)-exacerbated respiratory disease (NERD/N-ERD)[1] |
 | |
| Coated aspirin tablets | |
| Specialty | Rhinology, pulmonology, allergology |
| Symptoms | Adult-onset asthma, chronic rhinosinusitis with nasal polyps, NSAID hypersensitivity reactions |
| Usual onset | 20s to 40s, average age 35-36[2] |
| Duration | Long term |
| Causes | Chronic immune dysregulation of unknown origin |
| Diagnostic method | Symptoms and medical history; aspirin challenge[2] |
| Differential diagnosis | Allergic rhinitis, nonallergic rhinitis, nonallergic rhinitis with eosinophilia syndrome (NARES) |
| Management | Inhaled and intranasal corticosteroids, aspirin desensitization and therapy, biologics, sinus surgery, diet, antileukotrienes |
| Frequency | 0.3–0.9% (general population, US), ~7% of asthmatics[3] |
Aspirin-exacerbated respiratory disease (AERD), also called NSAID-exacerbated respiratory disease (N-ERD) or historically aspirin-induced asthma and Samter's Triad, is a long-term disease defined by three simultaneous symptoms: asthma, chronic rhinosinusitis with nasal polyps, and intolerance of aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs).[1][4] Compared to aspirin tolerant patients, AERD patients' asthma and nasal polyps are generally more severe. Reduction or loss of the ability to smell (hyposmia, anosmia) is extremely common, occurring in more than 90% of people with the disease.[5] AERD most commonly begins in early- to mid-adulthood and has no known cure. While NSAID intolerance is a defining feature of AERD, avoidance of NSAIDs does not affect the onset, development or perennial nature of the disease.[2]
The cause of the disease is a dysregulation of the arachidonic acid metabolic pathway and of various innate immune cells, though the initial cause of this dysregulation is currently unknown. This dysregulation leads to an imbalance of immune related molecules, including an overproduction of inflammatory compounds such as leukotriene E4 and an underproduction of anti-inflammatory mediators such as prostaglandin E2. This imbalance, among other factors, leads to chronic inflammation of the respiratory tract.[2]
A history of respiratory reactions to aspirin or others NSAIDs is sufficient to diagnose AERD in a patient that has both asthma and nasal polyps. However, diagnosis can be challenging during disease onset, as symptoms do not usually begin all at once. As symptoms appear, AERD may be misdiagnosed as simple allergic or nonallergic rhinitis or adult-onset asthma alone. It is only once the triad of symptoms are present that the diagnosis of AERD can be made.[5][2][6]
As there is no cure, treatment of AERD revolves around managing the symptoms of the disease. Corticosteroids, surgery, diet modifications and monoclonal antibody-based drugs are all commonly used, among other treatment options. Paradoxically, daily aspirin therapy after an initial desensitization can also help manage symptoms.
Reactions to aspirin and other NSAIDs range in severity but almost always have a respiratory component; severe reactions can be life threatening. The symptoms of NSAID-induced reactions are hypersensitivity reactions rather than allergic reactions that trigger other allergen-induced asthma, rhinitis, or hives. AERD is not considered an autoimmune disease, but rather a chronic immune dysregulation.[2][7] EAACI/WHO classifies the syndrome as one of five types of NSAID hypersensitivity.
Signs and symptoms
AERD affects an estimated 0.3–0.9% of the general population in the US, including around 7% of all asthmatics, about 14% of adults with severe asthma, and ~5-10% of patients with adult onset asthma.[2][3][8] AERD is uncommon among children, with around 6% of patients, predominantly female, reporting disease onset during childhood.[9] It is more prevalent among women by up to a 2:1 margin, usually begins in the patient's twenties to forties, with mean age of onset around 35.[2][10][11] AERD patients may not have any allergies, though allergies are significantly more common in AERD patients than the general population. While AERD has been found to affect essentially all ethnicities, it is less common in parts of Asia where nasal polyps caused by type 2 inflammation are relatively more rare.[5]
While disease progression varies, most commonly the first symptom is rhinitis (inflammation or irritation of the nasal mucosa), which may manifest as sneezing, runny nose, or congestion. The disorder typically progresses to asthma, then nasal polyposis, with aspirin sensitivity coming last. Hyposmia or anosmia—reduction or loss of the ability to smell—are reported in more than 90% of patients, as inflammation within the nose and sinuses likely reaches the olfactory receptors.[5]
Reactions to NSAIDs range in severity and expression. Onset is usually relatively rapid, with a mean time of around one hour after ingestion, though reactions as late as three hours have been reported. Respiratory reactions are essentially universal, with bronchoconstriction occurring in close to 90% of patients and nasal congestion and rhinorrhea occurring in more than 40%. Other symptoms include urticaria (hives), flushing, angioedema and hypotension. Gastrointestinal reactions have also been reported in a subset of patients, and may be difficult to treat. Factors that affect reaction severity include NSAID dosage, underlying asthma control, leukotriene modifier usage and the state of the patient's nasal polyps.[5]
In addition to aspirin, patients also react to other NSAIDs such as ibuprofen, and to any medication that inhibits the cyclooxygenase-1 (COX-1) enzyme, although paracetamol (acetaminophen) in low doses is generally considered safe. Selective COX-2 inhibitor NSAIDs that do not block COX-1, such as the celecoxib and rofecoxib, also are regarded as safe.[5] Nonetheless, recent studies do find that these types of drugs, e.g. acetaminophen and celecoxib, may trigger adverse reactions in these patients; caution is recommended in using any COX inhibitors.[12] In addition to aspirin and NSAIDs, consumption of even small amounts of alcohol also produces uncomfortable respiratory reactions in many patients.[13]
Causes and Pathophysiology
The reason for onset of AERD is currently unknown. Allergic reaction to the superantigen of Staphylococcus aureus, chronic viral infection and autoimmune mechanisms have been theorized, among others, though there is not sufficient evidence to support any specific theory. No strong genetic predisposition to or basis of AERD has been found, and familial AERD is rare. In addition, there is no relationship between past use of NSAIDs and onset of AERD[2]
AERD is generally thought to have two major components contributing to disease pathogenesis: abnormalities in the arachidonic acid metabolic cascade and dysregulation of various innate immune cells. These two components feed into each other in a highly complex negative cycle of increasing inflammation and dysregulation that is still under active research.[7][14]
Arachidonic acid cascade dysregulation
AERD is associated with an aberrant arachidonic acid metabolism that leads to changes in levels of two major classes of eicosanoids, specifically certain cysteinyl leukotrienes (cysLTs) and prostaglandins. Notably, reduced prostaglandin E2 (PGE2) decreases inhibition of 5-lipoxygenase (5-LO), causing increased conversion of arachidonic acid into leukotriene A4 (LTA4). LTA4 is converted into leukotriene C4 (LTC4), which itself is converted into leukotriene D4 (LTD4) and leukotriene E4 (LTE4), both powerful bronchoconstrictors. In contrast to PGE2, AERD patients show significantly higher levels of prostaglandin D2 (PGD2), which exerts pro-inflammatory effects via its recruitment of eosinophils and type 2 helper T cells (TH2) cells in addition to its direct bronchoconstrictive action.[14][15]
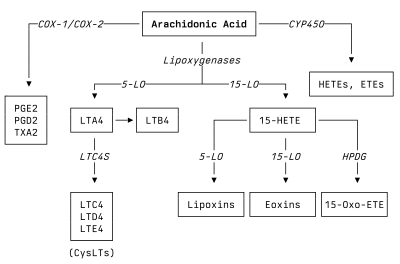
The exact mechanism by which aspirin and other COX-1 inhibitors lead to acute respiratory reactions is still under investigation. AERD patients exhibit a seemingly paradoxical response to COX-1 inhibition, as it leads to greatly increased PGD2 and LTE4 levels, instead of the expected decrease in PGD2 and relative lack of change in LTE4. However, given that COX-1 catalyzes the formation of PGE2, a leading explanation is that patients have an increased dependence on PGE2 and its corresponding receptor (EP2) to prevent inflammatory mediator release from mast cells. When COX-1 is inhibited, the decreased PGE2 production leads to mast cell degranulation and release of LTC4 and PGD2, which leads to respiratory symptom exacerbation.[14][16]
Patients with AERD also show increased expression of leukotriene C4 synthase (LTC4S), which converts LTA4 into LTC4. Platelets, which express LTC4S and generate LTC4 when attached to 5-LO-expressing leukocytes (including eosinophils), are also implicated in disease pathogenesis as well as acute aspirin-induced exacerbations. Additionally, after aspirin or other NSAID exposure, AERD patients generally become desensitized and tolerate a second exposure for around one week, which lines up with the half life of circulating platelets.[15][16]
Additional downstream products of arachidonic acid such as 15-lipoxygenase (15-LO) produced 15-HETE and 15-Oxo-ETE are significantly elevated in nasal polyps from AERD patients while other products like anti-inflammatory lipoxins are reduced. It's possible that increased 15-LO activity and preferential conversion of arachidonic acid into 15-Oxo-ETE and eoxins over lipoxins contributes to inflammation in AERD.[14][17]
Innate immune cells
Various innate immune cells also appear to play important roles in AERD pathogenesis. Eosinophils, mast cells, basophils and type 2 innate lymphoid (ILC2) cells have all been found at increased levels in the nasal polyps of AERD patients and appear to be part of the negative cycle of inflammation in AERD.[7]
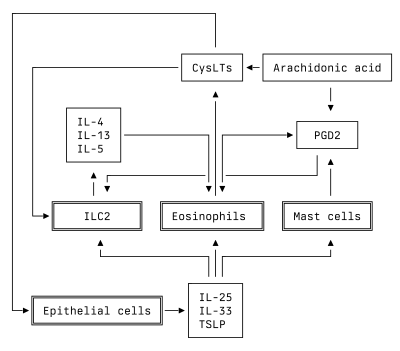
ILC2 cells are activated by CysLTs and PGD2 in addition to a class of cytokines called alarmins that are released by epithelial cells, including IL-25, IL-33 and thymic stromal lymphopoietin (TSLP). Strongly activated ILC2s release IL-4, IL-5 and IL-13. These cytokines lead to increased eosinophil recruitment, excessive mucus production via goblet cells, and promotion of TH2 and immunoglobulin E responses. These responses cause the epithelial cells to release more cytokines and inflammatory molecules, creating a feed-forward negative cycle of increasing inflammation.[7][16]
Eosinophils are also activated by ILC2-released IL-5 and epithelial-cell released IL-33, causing them to release more CysLTs and PGD2, which in turn further active ILC2. Likewise, mast cells are also activated by epithelial-cell released IL-25, IL-33 and TSLP, leading to further CysLT and PGD2 production.[7]
Basophils, which are degranulated in AERD nasal polyps, also appear to be important sources of IL-4 and IL-13.[7][14] In addition to activating immune cells, IL-4 and IL-13 have been shown to significantly increase 15-LO activity, further playing into the cycle of dysregulation and disease.[17]
Diagnosis
Diagnosis of AERD can be difficult, as symptoms develop over time and can often be attributed to allergies, common asthma, and/or nonallergic rhinitis. AERD is generally diagnosed based on a patient's medical history, however an oral aspirin challenge at a specialized facility is considered the most definitive method of diagnosis.[2]
Patients are considered candidates for an AERD diagnosis if they meet the following three points:
- History of adverse reactions to aspirin or other NSAIDs
- Reduced ability to smell (hyposmia or anosmia)
- History of rhinosinusitis and nasal polyps
Further, if a patient meets two or more of the following criteria, then an AERD diagnosis is strongly considered:[2]
- Moderate or severe asthma
- Asthma with an intractable cough
- Onset of asthma after adolescence
- A weakly atopic disposition
- 10% or greater increase in peripheral eosinophilia
High urinary leukotriene E4 (uLTE4) concentration is also a sign of AERD, especially when noted in conjunction with the criteria listed above due. High uLTE4 concentration alone cannot be used to diagnose AERD, however it may be possible to rule out AERD in patients without high uLTE4 due to its strong negative predictive value.[18] Urinary LTE4 concentration is generally around 3 to 5 times higher in patients with AERD that it is in those with aspirin-tolerant asthma, and increases 2 to 30 fold during an aspirin challenge test.[2]
Management
Medication
Since nasal polyps have been identified as an important source of inflammatory compounds in AERD, much effort goes into the prevention of polyp growth and control of sinus symptoms in general. There is evidence supporting four different long-term pharmacological treatments to this end: intra-nasal corticosteroids, aspirin desensitization and therapy, a range of biologic medicines, and antileukotrienes.[19][20] Each treatment has benefits and drawbacks, so no one option can be recommended for all patients. Asthma symptoms, if not controlled via biologics or other means, are managed with standard asthma treatments such as inhaled corticosteroids and long-acting beta-agonists.[2]
Despite optimal medical management, many patients continue to require oral steroid medications to alleviate asthma and chronic nasal congestion.[21]
Intra-nasal corticosteroids
Common corticosteroids such as fluticasone or budesonide are often used as a first line treatment for AERD. They can be delivered topically to the nasal and sinus mucosa via a variety of methods, such as nasal spray, rinse, drops, stents and exhalation delivery systems. Overall effectiveness is low-to-moderate, but wide availability and low cost make this a widely used treatment option.[19][22] Stent, spray and exhalation delivery systems are generally among the most beneficial depending on outcome measured, while no major differences in adverse effects have been measured between delivery methods.[19][22]
Aspirin desensitization and therapy
Avoidance of NSAID medications will not stop the progression of the disease. However, one treatment option is desensitization to aspirin, undertaken at a clinic or hospital specializing in such treatment.[23] Patients who are desensitized then take a maintenance dose of aspirin daily to maintain their desensitization. The recommended maintenance dose for symptom control is 650 mg to 1300 mg aspirin daily.[24] While on daily aspirin, patients experience improved quality of life and reduced nasal symptoms, however, there is no improvement in smell compared to placebo and there is no reduction in the need for oral corticosteroids or rescue surgery.[25][19] Once desensitized to aspirin, most patients can safely take other NSAID medications again as long the daily maintenance dose is continued.[26]
Risk of adverse advents such as bleeding or gastrointestinal side effects is relatively high with daily aspirin therapy. Even a 81 mg daily aspirin regimen for cardiovascular benefits has been shown to increase risk of long-term bleeding,[27] so the significantly higher aspirin doses used for maintenance therapy are of some concern.[19] This is borne out in studies on AERD patients—compared against standard of care and biologic medicines, aspirin therapy has a significantly higher rate of adverse outcomes.[25]
Biologics

Various novel biologic monoclonal antibody medications that have come to market in recent years have been used to treat AERD including dupilumab, mepolizumab, omalizumab, and benralizumab.[28][29] Among treatment options, biologics have the highest certainty and magnitude of improvement effect. However, due to the high cost and systemic nature of biologics, some patients whose symptoms are sufficiently controlled with other treatments may prefer to avoid them or not qualify under stricter prescription guidelines.[19]
Among biologics and aspirin desensitization and therapy, dupilumab (Dupixent) was show to be the most effective across six different patient-important outcomes.[29][25] Dupilumab and omalizumab have been shown to increase aspirin tolerance in AERD patients, however mepolizumab does not appear to have this effect.[30][31] The mechanism through which dupilumab treats AERD and restores aspirin tolerance is not fully understood, but it is theorized that by blocking IL-4α, dupilumab increases expression of EP2, the receptor for PGE2, back to normal levels, normalizing COX function and PGE2 production. Low PGE2 production and activity appear to play a key role in AERD, as PGE2 prevents inflammatory mediator release from mast cells and inhibits 5-LO function, which decreases production of CysLTs.[31][32]
Antileukotrienes
Leukotrienes are a family of inflammatory mediators derived from arachidonic acid that include CysLTs implicated in AERD pathophysiology. Drugs that prevent leukotriene production, such as zileuton, and that block leukotriene receptors, such as montelukast and zafirlukast, have proven to be useful in treatment of nasal polyposis. However, there may be limited additional benefit when used in conjunction with intra-nasal corticosteroids.[20][33] In a large survey, AERD patients reported that zileuton was more effective at controlling their symptoms than montelukast. Despite this, zileuton remains less prescribed than montelukast, likely due to concerns around risk of liver enzyme elevation.[34]
Surgery
Often functional endoscopic sinus surgery is required to remove nasal polyps,[35] although they typically recur, particularly if aspirin desensitization is not undertaken. Approximately, 90% of patients have been shown to have recurrence of nasal polyps within five years after surgery, with 47% requiring revision surgery in the same time period.[36] A complete endoscopic sinus surgery followed by aspirin desensitization has been shown to reduce the need for revision surgeries.[37] Exact cause of nasal polyp formation is unknown, however, differential gene expression analysis of AERD nasal polyp epithelial cells versus AERD non polyp nasal mucosa revealed DMRT3 could be potentially involved in nasal polyp development in AERD patients. Furthermore, several genes are down-regulated, hinting at the de-differentiation phenomenon in AERD polyps.[38]
Diet
Low omega-6/high omega-3
Given that dysregulation of the arachidonic acid cascade has been implicated in AERD pathogenesis and that production of arachidonic acid and its downstream products is influenced by the interaction and metabolism of omega-3 and omega-6 essential fatty acids, dietary interventions targeting the two essential fatty acids are under study.
A diet low in omega-6 fatty acids and high in omega-3 fatty acids—the opposite of an average modern western diet—has been shown to reduce arachidonic acid precursors and increase eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). EPA and DHA are precursors for anti-inflammatory compounds that modulate leukotrienes, prostaglandins and thromboxanes that have been implicated in AERD pathogenesis.[39] Initial studies have shown that decreasing omega-6 intake and increasing omega-3 intake decrease urinary LTE4 and prostaglandin D2 levels and significantly improved overall symptoms.[40][41][42] AERD specialists routinely recommend this diet as a treatment option.[40]
Alcohol
The majority of those with aspirin exacerbated respiratory disease experience respiratory reactions to alcohol. One study found that 83% reported such reactions. Of those who had reactions, 75% had a sinus reaction (runny nose, nasal congestion) and 51% had a lower respiratory reaction (wheezing, shortness of breath).[13] The current theory on the cause of these reactions is that they may be related to polyphenols found in alcoholic beverages.[43] A 2017 study found that alcohol sensitive patients reacted to catechins in red wine, but not to resveratrol.[44] It has been suggested that steel fermented white wines and clear liquors may cause less of a reaction than other alcoholic beverages.[45] Desensitization to aspirin has been found to reduce reactions to alcohol.[46]
Dietary salicylates
Given that aspirin is a salicylate, specifically acetyl salicylic acid, research has gone into low-salicylate diets such as the Feingold diet to see if they benefit AERD patients. For example, a prospective randomized trial with 30 patients following a low-salicylate diet for six weeks demonstrated a clinically significant decrease in both subjective and objective scoring of severity of disease, but made note of the challenge for patients in following what is a fairly stringent diet.[47] Despite these findings, experts on the disease do not believe that dietary salicylates contribute to AERD symptoms.[48] Dietary salicylates do not significantly inhibit the COX-1 enzyme, which is the cause of AERD reactions. One confounding factor in the study that showed a benefit from avoidance of dietary salicylates is that a low salicylate diet involves eliminating wine and beer. The majority of AERD patients react to wine and beer for reasons that do not involve their salicylate content.[13] There is also a strong placebo effect involved with any dietary intervention. In contrast to aspirin, dietary salicylates are not acetylated and therefore do not block cyclooxygenases and hence, there is no rationale why a low salicylate diet would be beneficial for AERD patients.[49]
Alternate and related names
- Aspirin-induced asthma
- Aspirin-intolerant asthma
- NSAID-exacerbated respiratory disease (NERD)
- Samter's triad (named for Max Samter)
- Leukotriene associated hypersensitivity[50]
- Acetylsalicylic acid triad[51]
- Widal's triad (named for Georges-Fernand Widal)
- Francis' triad
- Aspirin triad
- Aspirin-induced asthma and rhinitis (AIAR)[52]
History
The first adverse reactions to aspirin were described in 1902 in Germany, only four years after aspirin's commercial introduction.[53] The first published report of an aspirin-induced asthma attack was in 1911.[54] Initial reports on the linkage between asthma, aspirin, and nasal polyposis were made by Georges-Fernand Widal et al. in 1922.[55] Further studies were conducted by Samter and Beers in reports published in 1968, which brought full clinical characterization.[56][57] The recognition Samter brought to the disease through his studies led to it being called "Samter's triad", although today "aspirin-exacerbated respiratory disease" is preferred to better reflect the progressive nature of the condition even when patients abstain from NSAIDs.[57][4]
See also
References
- 1 2 Kowalski ML, Asero R, Bavbek S, Blanca M, Blanca-Lopez N, Bochenek G, et al. (October 2013). "Classification and practical approach to the diagnosis and management of hypersensitivity to nonsteroidal anti-inflammatory drugs". Allergy. 68 (10): 1219–1232. doi:10.1111/all.12260. PMID 24117484. S2CID 32169451.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Taniguchi M, Mitsui C, Hayashi H, Ono E, Kajiwara K, Mita H, et al. (July 2019). "Aspirin-exacerbated respiratory disease (AERD): Current understanding of AERD". Allergology International. 68 (3): 289–295. doi:10.1016/j.alit.2019.05.001. PMID 31235242. S2CID 195356657.
- 1 2 Li KL, Lee AY, Abuzeid WM (March 2019). "Aspirin Exacerbated Respiratory Disease: Epidemiology, Pathophysiology, and Management". Medical Sciences. 7 (3): 45. doi:10.3390/medsci7030045. PMC 6473909. PMID 30884882.
- 1 2 Kennedy JL, Stoner AN, Borish L (November 2016). "Aspirin-exacerbated respiratory disease: Prevalence, diagnosis, treatment, and considerations for the future". American Journal of Rhinology & Allergy. 30 (6): 407–413. doi:10.2500/ajra.2016.30.4370. PMC 5108840. PMID 28124651.
- 1 2 3 4 5 6 Haque R, White AA, Jackson DJ, Hopkins C (August 2021). "Clinical evaluation and diagnosis of aspirin-exacerbated respiratory disease". The Journal of Allergy and Clinical Immunology. 148 (2): 283–291. doi:10.1016/j.jaci.2021.06.018. PMID 34364538. S2CID 236958386.
- ↑ O'Brien EK, Jerschow E, Divekar RD (October 2023). "Management of Aspirin-Exacerbated Respiratory Disease: What Does the Future Hold?". Otolaryngologic Clinics of North America. doi:10.1016/j.otc.2023.09.006. PMID 37833102. S2CID 264093648.
- 1 2 3 4 5 6 Eid R, Yan CH, Stevens W, Doherty TA, Borish L (August 2021). "Innate immune cell dysregulation drives inflammation and disease in aspirin-exacerbated respiratory disease". The Journal of Allergy and Clinical Immunology. 148 (2): 309–318. doi:10.1016/j.jaci.2021.06.016. PMC 8363117. PMID 34364539.
- ↑ Rajan JP, Wineinger NE, Stevenson DD, White AA (March 2015). "Prevalence of aspirin-exacerbated respiratory disease among asthmatic patients: A meta-analysis of the literature". The Journal of Allergy and Clinical Immunology. 135 (3): 676–81.e1. doi:10.1016/j.jaci.2014.08.020. PMID 25282015.
- ↑ Bensko JC, McGill A, Palumbo M, Cahill KN, Laidlaw TM (September 2022). "Pediatric-onset aspirin-exacerbated respiratory disease: Clinical characteristics, prevalence, and response to dupilumab". The Journal of Allergy and Clinical Immunology. In Practice. 10 (9): 2466–2468. doi:10.1016/j.jaip.2022.05.016. PMID 35643277. S2CID 249074081.
- ↑ Welch KC, Patel Z (2015-01-20). "Aspirin Desensitization". American Rhinologic Society. Archived from the original on 2018-12-27.
- ↑ Chen BS, Virant FS, Parikh SR, Manning SC (February 2013). "Aspirin sensitivity syndrome (Samter's Triad): an unrecognized disorder in children with nasal polyposis". International Journal of Pediatric Otorhinolaryngology. 77 (2): 281–283. doi:10.1016/j.ijporl.2012.10.017. PMID 23149179.
- ↑ Kim YJ, Lim KH, Kim MY, Jo EJ, Lee SY, Lee SE, et al. (March 2014). "Cross-reactivity to Acetaminophen and Celecoxib According to the Type of Nonsteroidal Anti-inflammatory Drug Hypersensitivity". Allergy, Asthma & Immunology Research. 6 (2): 156–162. doi:10.4168/aair.2014.6.2.156. PMC 3936045. PMID 24587953.
- 1 2 3 Cardet JC, White AA, Barrett NA, Feldweg AM, Wickner PG, Savage J, et al. (2014). "Alcohol-induced respiratory symptoms are common in patients with aspirin exacerbated respiratory disease". The Journal of Allergy and Clinical Immunology. In Practice. 2 (2): 208–13. doi:10.1016/j.jaip.2013.12.003. PMC 4018190. PMID 24607050.
- 1 2 3 4 5 Sehanobish E, Asad M, Jerschow E (February 2022). "New concepts for the pathogenesis and management of aspirin-exacerbated respiratory disease". Current Opinion in Allergy and Clinical Immunology. 22 (1): 42–48. doi:10.1097/ACI.0000000000000795. PMC 8702488. PMID 34739410.
- 1 2 Narayanankutty A, Reséndiz-Hernández JM, Falfán-Valencia R, Teran LM (May 2013). "Biochemical pathogenesis of aspirin exacerbated respiratory disease (AERD)". Clinical Biochemistry. 46 (7–8): 566–578. doi:10.1016/j.clinbiochem.2012.12.005. PMID 23246457.
- 1 2 3 Mullol J, Boyce J, Dahlén SE, Dahlén B, Picado C, Bobolea I (November 2021). "Eicosanoid dysregulation and type 2 inflammation in AERD". The Journal of Allergy and Clinical Immunology. 148 (5): 1157–1160. doi:10.1016/j.jaci.2021.08.015. PMID 34464635. S2CID 237374571.
- 1 2 Lyly A, Laidlaw TM, Lundberg M (2021). "Pathomechanisms of AERD-Recent Advances". Frontiers in Allergy. 2: 734733. doi:10.3389/falgy.2021.734733. PMC 8974777. PMID 35387030.
- ↑ Bochenek G, Stachura T, Szafraniec K, Plutecka H, Sanak M, Nizankowska-Mogilnicka E, Sladek K (March 2018). "Diagnostic Accuracy of Urinary LTE4 Measurement to Predict Aspirin-Exacerbated Respiratory Disease in Patients with Asthma". The Journal of Allergy and Clinical Immunology. In Practice. 6 (2): 528–535. doi:10.1016/j.jaip.2017.07.001. PMID 28888846.
- 1 2 3 4 5 6 Kim SL, Rank MA, Peters AT (December 2022). "The chronic rhinosinusitis practice parameter". Annals of Allergy, Asthma & Immunology. 131 (3): 307–310. doi:10.1016/j.anai.2022.12.022. PMID 36538974. S2CID 254849277.
- 1 2 Wentzel JL, Soler ZM, DeYoung K, Nguyen SA, Lohia S, Schlosser RJ (November 2013). "Leukotriene antagonists in nasal polyposis: a meta-analysis and systematic review". American Journal of Rhinology & Allergy. 27 (6): 482–489. doi:10.2500/ajra.2013.27.3976. PMC 3899527. PMID 24274224.
- ↑ Szczeklik A, Nizankowska E, Duplaga M (September 2000). "Natural history of aspirin-induced asthma. AIANE Investigators. European Network on Aspirin-Induced Asthma". The European Respiratory Journal. 16 (3): 432–436. doi:10.1034/j.1399-3003.2000.016003432.x. PMID 11028656.
- 1 2 Bognanni A, Chu DK, Rank MA, Bernstein J, Ellis AK, Golden D, et al. (December 2022). "Topical corticosteroids for chronic rhinosinusitis with nasal polyposis: GRADE systematic review and network meta-analysis". The Journal of Allergy and Clinical Immunology. 150 (6): 1447–1459. doi:10.1016/j.jaci.2022.07.023. PMID 35970310. S2CID 251547875.
- ↑ Waldram JD, Simon RA (November 2016). "Performing Aspirin Desensitization in Aspirin-Exacerbated Respiratory Disease". Immunology and Allergy Clinics of North America. 36 (4): 693–703. doi:10.1016/j.iac.2016.06.006. PMID 27712764.
- ↑ Lee JY, Simon RA, Stevenson DD (January 2007). "Selection of aspirin dosages for aspirin desensitization treatment in patients with aspirin-exacerbated respiratory disease". The Journal of Allergy and Clinical Immunology. 119 (1): 157–164. doi:10.1016/j.jaci.2006.09.011. PMID 17208597.
- 1 2 3 Oykhman P, Paramo FA, Bousquet J, Kennedy DW, Brignardello-Petersen R, Chu DK (April 2022). "Comparative efficacy and safety of monoclonal antibodies and aspirin desensitization for chronic rhinosinusitis with nasal polyposis: A systematic review and network meta-analysis". The Journal of Allergy and Clinical Immunology. 149 (4): 1286–1295. doi:10.1016/j.jaci.2021.09.009. PMID 34543652. S2CID 237584489.
- ↑ Pleskow WW, Stevenson DD, Mathison DA, Simon RA, Schatz M, Zeiger RS (January 1982). "Aspirin desensitization in aspirin-sensitive asthmatic patients: clinical manifestations and characterization of the refractory period". The Journal of Allergy and Clinical Immunology. 69 (1 Pt 1): 11–19. doi:10.1016/0091-6749(82)90081-1. PMID 7054250.
- ↑ Davidson KW, Barry MJ, Mangione CM, Cabana M, Chelmow D, Coker TR, et al. (April 2022). "Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force Recommendation Statement". JAMA. 327 (16): 1577–1584. doi:10.1001/jama.2022.4983. PMID 35471505. S2CID 248390304.
- ↑ Tuttle KL, Buchheit KM, Schneider T, Hsu Blatman KS, Barrett NA, Laidlaw TM, Cahill KN (February 2018). "A pragmatic analysis of mepolizumab in patients with aspirin-exacerbated respiratory disease". Journal of Allergy and Clinical Immunology. 141 (2): AB168. doi:10.1016/j.jaci.2017.12.537.
- 1 2 Wangberg H, Spierling Bagsic SR, Osuna L, White AA (February 2022). "Appraisal of the Real-World Effectiveness of Biologic Therapies in Aspirin-Exacerbated Respiratory Disease". The Journal of Allergy and Clinical Immunology. In Practice. 10 (2): 478–484.e3. doi:10.1016/j.jaip.2021.09.030. PMC 8837666. PMID 34597850.
- ↑ Mustafa SS, Vadamalai K (June 2021). "Dupilumab increases aspirin tolerance in aspirin-exacerbated respiratory disease". Annals of Allergy, Asthma & Immunology. 126 (6): 738–739. doi:10.1016/j.anai.2021.03.010. PMID 33746062. S2CID 232308870.
- 1 2 Picado C, Mullol J, Roca-Ferrer J (September 2022). "Mechanisms by which dupilumab normalizes eicosanoid metabolism and restores aspirin-tolerance in AERD: A hypothesis". The Journal of Allergy and Clinical Immunology. 151 (2): 310–313. doi:10.1016/j.jaci.2022.09.012. PMID 36126795. S2CID 252363143.
- ↑ Buchheit KM, Sohail A, Hacker J, Maurer R, Gakpo D, Bensko JC, et al. (August 2022). "Rapid and sustained effect of dupilumab on clinical and mechanistic outcomes in aspirin-exacerbated respiratory disease". The Journal of Allergy and Clinical Immunology. 150 (2): 415–424. doi:10.1016/j.jaci.2022.04.007. PMC 9378638. PMID 35460728.
- ↑ San Nicoló M, Habermann N, Havel M (2020). "AERD Associated Nasal Polyposis: Efficacy of Postoperative Antileukotriene Therapy in Comparison with Aspirin Desensitization. A Retrospective Study". International Archives of Allergy and Immunology. 181 (10): 790–798. doi:10.1159/000508708. PMID 32777782. S2CID 221099029.
- ↑ Ta V, White AA (September 2015). "Survey-Defined Patient Experiences With Aspirin-Exacerbated Respiratory Disease". The Journal of Allergy and Clinical Immunology. In Practice. 3 (5): 711–718. doi:10.1016/j.jaip.2015.03.001. PMID 25858054.
- ↑ McMains KC, Kountakis SE (2006). "Medical and surgical considerations in patients with Samter's triad". American Journal of Rhinology. 20 (6): 573–576. doi:10.2500/ajr.2006.20.2913. PMID 17181095. S2CID 33480314.
- ↑ Mendelsohn D, Jeremic G, Wright ED, Rotenberg BW (March 2011). "Revision rates after endoscopic sinus surgery: a recurrence analysis". The Annals of Otology, Rhinology, and Laryngology. 120 (3): 162–166. doi:10.1177/000348941112000304. PMID 21510141. S2CID 26696888.
- ↑ Adappa ND, Ranasinghe VJ, Trope M, Brooks SG, Glicksman JT, Parasher AK, et al. (January 2018). "Outcomes after complete endoscopic sinus surgery and aspirin desensitization in aspirin-exacerbated respiratory disease". International Forum of Allergy & Rhinology. 8 (1): 49–53. doi:10.1002/alr.22036. PMID 29105347. S2CID 5811563.
- ↑ Priyadharshini, V.S.; Jiménez-Chobillon, M.A.; de Graaf, J.; Porras Gutiérrez de Velasco, R.; Gratziou, C.; Ramírez-Jiménez, F.; Teran, L.M. Transcriptome Analysis Identifies Doublesex and Mab-3 Related Transcription Factor (DMRT3) in Nasal Polyp Epithelial Cells of Patients Suffering from Non-Steroidal Anti-Inflammatory Drug-Exacerbated Respiratory Disease (AERD). Biomolecules 2021, 11, 1092. https://doi.org/10.3390/biom11081092
- ↑ Modena BD, White AA (May 2018). "Can Diet Modification Be an Effective Treatment in Aspirin-Exacerbated Respiratory Disease?". The Journal of Allergy and Clinical Immunology. In Practice. 6 (3): 832–833. doi:10.1016/j.jaip.2017.11.043. PMC 6455762. PMID 29747986.
- 1 2 Laidlaw TM (January 2019). "Clinical updates in aspirin-exacerbated respiratory disease". Allergy and Asthma Proceedings. 40 (1): 4–6. doi:10.2500/aap.2019.40.4188. PMC 6313255. PMID 30582489.
- ↑ Schneider TR, Johns CB, Palumbo ML, Murphy KC, Cahill KN, Laidlaw TM (2018). "Dietary Fatty Acid Modification for the Treatment of Aspirin-Exacerbated Respiratory Disease: A Prospective Pilot Trial". The Journal of Allergy and Clinical Immunology. In Practice. 6 (3): 825–831. doi:10.1016/j.jaip.2017.10.011. PMC 5945343. PMID 29133219.
- ↑ Healy E, Newell L, Howarth P, Friedmann PS (December 2008). "Control of salicylate intolerance with fish oils". The British Journal of Dermatology. 159 (6): 1368–1369. doi:10.1111/j.1365-2133.2008.08830.x. PMID 18795922. S2CID 25041594.
- ↑ Payne SC (September 2014). "Re: Alcohol-induced respiratory symptoms are common in patients with aspirin exacerbated respiratory disease". The Journal of Allergy and Clinical Immunology. In Practice. 2 (5): 644. doi:10.1016/j.jaip.2014.05.003. PMID 25213072.
- ↑ Payne SC, Peters RD, Negri JA, Steinke JW, Borish L (February 2017). "Activation of Basophils and Eosinophils by EtOH in Alcohol Sensitive Patients with CRS and Asthma". Journal of Allergy and Clinical Immunology. 139 (2): AB90. doi:10.1016/j.jaci.2016.12.246.
- ↑ "Wine and Beer May Make Your Lungs and Sinuses Worse". www.aaaai.org. American Academy of Allergy Asthma & Immunology. August 3, 2018.
- ↑ Ta V, White AA (July 2018). "Survey-Defined Patient Experiences With Aspirin-Exacerbated Respiratory Disease". The Journal of Allergy and Clinical Immunology. In Practice. 3 (5): 711–718. doi:10.1016/j.jaip.2015.03.001. PMID 25858054.
- ↑ Sommer DD, Rotenberg BW, Sowerby LJ, Lee JM, Janjua A, Witterick IJ, et al. (April 2016). "A novel treatment adjunct for aspirin exacerbated respiratory disease: the low-salicylate diet: a multicenter randomized control crossover trial". International Forum of Allergy & Rhinology. 6 (4): 385–391. doi:10.1002/alr.21678. PMID 26751262. S2CID 205339377.
- ↑ Modena BD, White AA (2018). "Can Diet Modification Be an Effective Treatment in Aspirin-Exacerbated Respiratory Disease?". The Journal of Allergy and Clinical Immunology. In Practice. 6 (3): 832–833. doi:10.1016/j.jaip.2017.11.043. PMC 6455762. PMID 29747986.
- ↑ "A Low Salicylate Diet for AERD (Samter's Triad)". The Samter's Society.
- ↑ Lewis C (2017). "Leukotriene Associated Hypersensitivity". Enteroimmunology: A Guide to the Prevention and Treatment of Chronic Inflammatory Disease. Carrabelle Florida: Psy Press. pp. 148–58. ISBN 978-1-938318-06-1.
- ↑ Amar YG, Frenkiel S, Sobol SE (February 2000). "Outcome analysis of endoscopic sinus surgery for chronic sinusitis in patients having Samter's triad". The Journal of Otolaryngology. 29 (1): 7–12. PMID 10709165.
- ↑ Bochenek G, Bánska K, Szabó Z, Nizankowska E, Szczeklik A (March 2002). "Diagnosis, prevention and treatment of aspirin-induced asthma and rhinitis". Current Drug Targets. Inflammation and Allergy. 1 (1): 1–11. doi:10.2174/1568010023345011. PMID 14561202.
- ↑ "Anaphylactoid reaction to aspirin (1902)". Allergy Proceedings. 11 (5): 249–250, discussion 251–252. 1990. PMID 2258047.
- ↑ Saygin D, Tabib T, Bittar HE, Valenzi E, Sembrat J, Chan SY, et al. (1911-04-29). "Transcriptional profiling of lung cell populations in idiopathic pulmonary arterial hypertension". Pulmonary Circulation. 10 (1): 1262. doi:10.1177/2045894020908782. PMC 7052475. PMID 32166015.
- ↑ Widal F, Abrami P, Lermoyez J (1922). "Anaphylaxie et idiosyncraise" [Anaphylaxis and idiosyncrasy]. La Presse Médicale (in French). 30 (18): 189–93.
- ↑ Samter M, Beers RF (May 1968). "Intolerance to aspirin. Clinical studies and consideration of its pathogenesis". Annals of Internal Medicine. 68 (5): 975–983. doi:10.7326/0003-4819-68-5-975. PMID 5646829.
- 1 2 Kim SD, Cho KS (June 2018). "Samter's Triad: State of the Art". Clinical and Experimental Otorhinolaryngology. 11 (2): 71–80. doi:10.21053/ceo.2017.01606. PMC 5951071. PMID 29642688.