| Pott's disease | |
|---|---|
 | |
| Tuberculosis of the spine in an Egyptian mummy | |
| Specialty | Rheumatology |
| Symptoms | Pott's spine, tuberculous spondylitis, spinal tuberculosis |
| Diagnostic method | Radiograph, Bone scan, MRI |
| Named after | Percivall Pott |
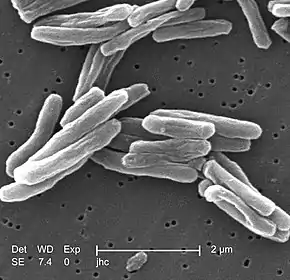
Pott's disease, or Pott disease, named for British surgeon Percivall Pott who first described the symptoms in 1799,[1] is tuberculosis of the spine,[2][3] usually due to haematogenous spread from other sites, often the lungs. The lower thoracic and upper lumbar vertebrae areas of the spine are most often affected.
It causes a kind of tuberculous arthritis of the intervertebral joints. The infection can spread from two adjacent vertebrae into the adjoining intervertebral disc space. If only one vertebra is affected, the disc is normal, but if two are involved, the disc, which is avascular, cannot receive nutrients, and collapses. In a process called caseous necrosis, the disc tissue dies, leading to vertebral narrowing and eventually to vertebral collapse and spinal damage. A dry soft-tissue mass often forms and superinfection is rare.
Spread of infection from the lumbar vertebrae to the psoas muscle, causing abscesses, is not uncommon.[4]
Diagnosis
- Blood tests
- Complete blood count: leukocytosis
- Elevated erythrocyte sedimentation rate: >100 mm/h
- Tuberculin skin test
- Tuberculin skin test (purified protein derivative [PPD]) results are positive in 84–95% of patients with Pott disease who are not infected with HIV.

- Radiographs of the spine
- Radiographic changes associated with Pott disease present relatively late. These radiographic changes are characteristic of spinal tuberculosis on plain radiography:
- Lytic destruction of anterior portion of vertebral body
- Increased anterior wedging
- Collapse of vertebral body
- Reactive sclerosis on a progressive lytic process
- Enlarged psoas shadow with or without calcification
- Additional radiographic findings may include:
- Vertebral end plates are osteoporotic
- Intervertebral disks may be shrunken or destroyed
- Vertebral bodies show variable degrees of destruction
- Fusiform paravertebral shadows suggest abscess formation
- Bone lesions may occur at more than one level
- Bone scan
- Computed tomography of the spine
- Bone biopsy
- MRI
Epidemiology
Half of the cases of musculoskeletal tuberculosis are Pott's Disease, of which 98% affect the anterior column. The disease can be attributed to 1.3 million deaths per year. There is a correlation between tuberculosis infections and cases of Pott's disease, as it's prevalent in areas where tuberculosis infections are common . Factors like socioeconomic status, habits, medical history, and interactions with people with tuberculosis can influence the rate of diagnosis.
Underdeveloped countries have a higher incidence rate of Pott's disease as it's associated with less ventilated rooms, crowded spaces, poorer hygiene, and less access to healthcare facilities. Increasing food security, reducing poverty, and improving living and working conditions will help to prevent infection and generally enhance the care of those sick.
Pott's disease is more common in the working-age population. It is becoming increasingly prevalent in older adults due to increased life expectancies, increased immunosuppressant use, chronic diseases like diabetes, and a rise in drug-resistant tuberculosis strains. In older populations, the disease is often misdiagnosed, often being disregarded for other degenerative diseases. Children's spines contain more cartilage, increasing the effect of spinal deformations caused by the disease.
Multidrug resistant tuberculosis poses a threat to people with Pott's disease, making it difficult to determine infection in people because of the paucibacillary symptoms of the disease. Cases of tuberculosis have been on the decline; however, infections of multidrug resistant tuberculosis have remained constant since the 1990s.
Prevention
Controlling the spread of tuberculosis infection can prevent tuberculous spondylitis and arthritis. Patients who have a positive PPD test (but not active tuberculosis) may decrease their risk by properly taking medicines to prevent tuberculosis. To effectively treat tuberculosis, patients must take their medications exactly as prescribed.[2]
Management
- Nonoperative:
- antituberculous drugs
- Analgesics
- Immobilization of the spine region using different types of braces and collars
- Physical therapy for pain-relieving modalities, postural education, and teaching a home-exercise program for strength and flexibility
- Surgery may be necessary, especially to drain spinal abscesses or debride bony lesions fully or to stabilize the spine. A 2007 review found just two randomized clinical trials with at least one-year follow-up that compared chemotherapy plus surgery with chemotherapy alone for treating people diagnosed with active tuberculosis of the spine. As such, no high-quality evidence exists, but the results of this study indicates that surgery should not be recommended routinely and clinicians have to selectively judge and decide on which patients to operate.[5]
- Thoracic spinal fusion with or without instrumentation as a last resort
Prognosis
- Paraplegia (so-called Pott's paraplegia)
- Vertebral collapse resulting in kyphosis
- Sinus formation
- Spinal cord compression
History
- Saint Gemma of Lucca had tuberculosis of the spine.
- English poets Alexander Pope and William Ernest Henley both had Pott disease.
- Anna Roosevelt Cowles, sister of President Theodore Roosevelt, had Pott disease.
- Søren Kierkegaard may have died from Pott disease, according to professor Kaare Weismann and literature scientist Jens Staubrand[6]
- Chick Webb, a swing-era drummer and band leader, was affected by tuberculosis of the spine as a child, which left him hunchbacked, and eventually caused his death.
- The Sicilian mafia boss Luciano Leggio had the disease and wore a brace.
- Italian writer, poet, and philosopher Giacomo Leopardi had the disease.
- It features prominently in the book This Is a Soul, which chronicles the work of American physician Rick Hodes in Ethiopia.
- Jane Addams, social activist and Nobel Peace Prize winner, had Pott disease.
- Willem Ten Boom, brother of Corrie Ten Boom, died of tuberculosis of the spine in December 1946.[7]
- Writer Max Blecher had Pott disease and wrote about the affliction.
- Marxist thinker and Communist leader Antonio Gramsci had Pott disease which, together with the bad conditions of his incarceration in fascist Italy during the 1930s, contributed to his death.
- Gavrilo Princip, who assassinated Archduke Franz Ferdinand of Austria, leading to World War I, died in prison of bone tuberculosis.
- English writer Denton Welch (1915–1948) died of spinal tuberculosis after being involved in a motor accident (1935) that irreparably damaged his spine.
- Louis Joseph, Dauphin of France, son of King Louis XVI and Marie Antoinette[8]
- George Mercer Dawson, Canadian surveyor, geologist and president of the Geological Society of America, had Pott's disease.
- Masaoka Shiki, Japanese poet, author and literary critic, had Pott's disease.
In works of literature
- Max Blecher's semi-autobiographical novel Inimi cicatrizate (1937) is about a young man named Emanuel who is afflicted with Pott disease in a sanatorium, as is the Radu Jude film Scarred Hearts (2016), loosely based on it.
- A. J. Cronin's story "Two Gentlemen of Verona," includes a character named Lucia with tuberculosis of spine.
- In William Golding's novel The Spire (1964), Jocelin, the dean who wanted a spire on his cathedral, probably dies as a result of the disease.
- Katharine Butler Hathaway's memoir The Little Locksmith (1943) is about the effects of spinal tuberculosis on her childhood and adult life.
- In Victor Hugo's Hunchback of Notre Dame (1831) the title character has a gibbus deformity similar to the type caused by spinal tuberculosis.
- In Henrik Ibsen's play A Doll's House (1879), Dr. Rank has "consumption of the spine."
- In Sergio Leone's film Once Upon a Time in the West (1968), Morton, the railroad magnate, has the disease and needs crutches to walk.
- In Ernest Poole's Pulitzer Prize-winning novel, His Family (1917), young Johnny Geer has a terminal case of Pott disease.
- In Edmund Wilson's Memoirs of Hecate County (1946), the novella "The Princess with the Golden Hair," has a character with Pott disease.
References
- ↑ Tuli, Surendar M. (June 22, 2013). "Historical aspects of Pott's disease (spinal tuberculosis) management". European Spine Journal. 22 (Suppl 4): 529–538. doi:10.1007/s00586-012-2388-7. PMC 3691412. PMID 22802129.
- 1 2 Garg, RK; Somvanshi, DS (2011). "Spinal tuberculosis: a review". The Journal of Spinal Cord Medicine. 34 (5): 440–54. doi:10.1179/2045772311Y.0000000023. PMC 3184481. PMID 22118251.
- ↑ "Pott Disease (Tuberculous [TB] Spondylitis): Background, Pathophysiology, Epidemiology". 18 February 2022. Retrieved 12 August 2023.
- ↑ Wong-Taylor, LA; Scott, AJ; Burgess, H (20 May 2013). "Massive TB psoas abscess". BMJ Case Reports. 2013: bcr2013009966. doi:10.1136/bcr-2013-009966. PMC 3670072. PMID 23696148.
- ↑ Jutte PC, van Loenhout-Rooyackers JH. Routine surgery in addition to chemotherapy for treating spinal tuberculosis. Cochrane Database of Systematic Reviews 2006, Issue 1. Art. No.: CD004532. DOI: 10.1002/14651858.CD004532.pub2. http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD004532.pub2/abstract
- ↑ Krasnik, Benjamin (2013). "Kierkegaard døde formentlig af Potts sygdom" (in Danish). Kristeligt Dagblad. Archived from the original on 2016-10-13. Retrieved 2016-10-02.
- ↑ The Hiding Place, Chapter: "Since Then"
- ↑ Covington, Richard. "Marie Antoinette". Smithsonian. Retrieved 2019-08-18.
External links
![]() Media related to Pott's disease at Wikimedia Commons
Media related to Pott's disease at Wikimedia Commons