Tubular carcinoma is a subtype of invasive ductal carcinoma of the breast.[2][3] More rarely, tubular carcinomas may arise in the pancreas[4] or kidney.[5] Most tubular carcinomas begin in the milk duct of the breast and spread to healthy tissue around it.[6][7]
Pathology
Although tubular carcinoma has been considered a special-type tumor,[lower-alpha 1] recent trend has been to classify it as a low-grade, invasive NOS carcinoma because there is a continuous spectrum from pure tubular carcinomas to mixed NOS[lower-alpha 2] carcinomas with tubular features, depending on the percentage of the lesion that displays tubular features.[10]: 647
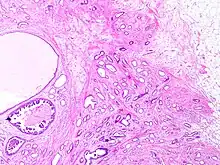
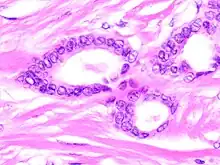
Histology
Tubular carcinomas are generally around 1 cm. or smaller, and are made up of tubules. They are usually low-grade.[2] Elastosis has been noted as common but is not present in all cases.[11]
Prevalence
Prevalence has previously been controversial, with contradictory reports from studies reporting either very low prevalence, or a high prevalence.[10] With the increasing availability of screening mammography, however, tubular carcinomas are being diagnosed earlier, and more recent studies suggest tubular carcinomas represent between 8% and 27% of all breast cancers.[2]
Prognosis
Tubular carcinoma is one of the histologic types of breast cancer with a more favorable outcome.[12]
See also
- Breast cancer classification
- Ductal carcinoma in situ – a common precancerous or Stage 0 breast cancer
- Invasive cribriform carcinoma of the breast – a rare breast cancer that consists of >50% cribriform histopathology but commonly has small or large areas (<50%) closely resembling tubular carcinoma histopathology.[13]
- Intraductal papillary mucinous neoplasm
- Invasive carcinoma of no special type
- Invasive lobular carcinoma
- Invasion (cancer)
Notes and references
- Notes
- ↑ Special-type tumor: such as mucinous and cribriform carcinomas.[8]
- ↑ NOS: of type "Not Otherwise Specified".[9]
- References
- 1 2 Image by Mikael Häggström, MD. Reference for typical features: Pragya Virendrakumar Jain, M.D., Julie M. Jorns, M.D. "Breast - Other invasive carcinoma subtypes, WHO classified - Tubular". Pathology Outlines.
{{cite web}}: CS1 maint: multiple names: authors list (link) Last author update: 23 March 2023 - 1 2 3 Hudis, Kenneth (22 June 2019). "IDC Type: Tubular Carcinoma of the Breast". Breastcancer.org. Retrieved 26 February 2022.
- ↑ Limaiem, Faten; Mlika, Mouna (2022). "Tubular Breast Carcinoma". StatPearls. StatPearls Publishing. PMID 31194380. Retrieved 3 March 2022.
- ↑ Chelliah, Adeline; Kalimuthu, Sangeetha; Chetty, Runjan (October 2016). "Intraductal tubular neoplasms of the pancreas: an overview". Ann Diagn Pathol. 24 (24:68–72): 68–72. doi:10.1016/j.anndiagpath.2016.04.009. PMID 27185640.
- ↑ Zhao, Ming; He, Xiang-lei; Teng, Xiao-dong (December 2015). "Mucinous tubular and spindle cell renal cell carcinoma: a review of clinicopathologic aspects". Diagnostic Pathology. 10 (1): 168. doi:10.1186/s13000-015-0402-1. PMC 4573286. PMID 26377921.
- ↑ Musser, Robert (2009). The P.I.N.K. Primer. Dog Ear Publishing. pp. 20–. ISBN 978-1-60844-176-1.
- ↑ Feng, Yixiao; Spezia, Mia; Huang, Shifeng; Yuan, Chengfu; Zeng, Zongyue; Zhang, Linghuan; Ji, Xiaojuan; Liu, Wei; Huang, Bo; Luo, Wenping; Liu, Bo; Lei, Yan; Du, Scott; Vuppalapati, Akhila; Luu, Hue H.; Haydon, Rex C.; He, Tong-Chuan; Ren, Guosheng (June 2018). "Breast cancer development and progression: Risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis". Genes & Diseases. 5 (2): 77–106. doi:10.1016/j.gendis.2018.05.001. PMC 6147049. PMID 30258937.
- ↑ "Understanding Your Pathology Report: Breast Cancer", Cancer.org, American Cancer Society, 2022, retrieved 26 February 2022
- ↑ "Farlex Partner Medical Dictionary". 2009. not otherwise specified. Retrieved 26 February 2022.
- 1 2 Stavros, A. Thomas (2004). Rapp, Cynthia L.; Parker, Steve H. (eds.). Breast Ultrasound. Lippincott Williams & Wilkins. pp. 647–649. ISBN 978-0-397-51624-7. OCLC 1065689596. p. 649:
A highly differentiated invasive carcinoma that forms well-defined tubules (containing epithelium, but no myoepithelium) and that have abundant desmoplastic fibrous stromal reaction between the tubules.
- ↑ Rosen, Paul Peter, ed. (2001). Rosen's Breast Pathology. Lippincott Williams & Wilkins. pp. 373–. ISBN 978-0-7817-2379-4. OCLC 1117861419.
- ↑ "Breast Cancer Treatment (Adult) (PDQ®)–Health Professional Version". National Cancer Institute. 20 January 2022. Retrieved 26 February 2022.
- ↑ Demir S, Sezgin G, Sari AA, Kucukzeybek BB, Yigit S, Etit D, Yazici A, Kucukzeybek Y (October 2021). "Clinicopathological analysis of invasive cribriform carcinoma of the breast, with review of the literature". Annals of Diagnostic Pathology. 54: 151794. doi:10.1016/j.anndiagpath.2021.151794. PMID 34325338.
Further reading
- Cserni, Gábor (March 2020). "Histological type and typing of breast carcinomas and the WHO classification changes over time". Pathologica. 112 (1): 25–41. doi:10.32074/1591-951X-1-20. PMC 8138497. PMID 32202537.
- Erber, Ramona; Hartmann, Arndt (August 2020). "Histology of Luminal Breast Cancer". Breast Care. Basel. 15 (4): 327–336. doi:10.1159/000509025. PMC 7490665. PMID 32982642.
- Sanders, Melinda A.; Mayer, Ingrid A.; Chakravarthy, Bapsi (3 March 2017). "22 Tubular Carcinoma of the Breast". In Raghavan, Derek; Ahluwalia, Manmeet S.; Blanke, Charles D.; et al. (eds.). Textbook of Uncommon Cancer (5 ed.). John Wiley & Sons. pp. 338–344. ISBN 978-1-119-19621-1. OCLC 1069570078.
- Zhang, Hanwen; Zhang, Ning (December 2020). "Special subtypes with favorable prognosis in breast cancer: A registry-based cohort study and network meta-analysis". Cancer Treatment Reviews. 91: 102–108. doi:10.1016/j.ctrv.2020.102108. PMID 33075683.