| Betacoronavirus viroporin | |||||||||
|---|---|---|---|---|---|---|---|---|---|
 | |||||||||
| Identifiers | |||||||||
| Symbol | bCoV_viroporin | ||||||||
| Pfam | PF11289 | ||||||||
| InterPro | IPR024407 | ||||||||
| |||||||||
ORF3a (previously known as X1 or U274)[2] is a gene found in coronaviruses of the subgenus Sarbecovirus, including SARS-CoV[3][2] and SARS-CoV-2.[1][4] It encodes an accessory protein about 275 amino acid residues long, which is thought to function as a viroporin.[1] It is the largest accessory protein[2][4] and was the first of the SARS-CoV accessory proteins to be described.[3]
Comparative genomics
ORF3a is well conserved within the subgenus Sarbecovirus.[3][2] The protein has 73% sequence identity between SARS-CoV (274 residues) and SARS-CoV-2 (275 residues).[1] Within the ORF3a open reading frame there are several overlapping genes in the genome: ORF3a, ORF3b, and (in SARS-CoV-2 only) ORF3c. In SARS-CoV-2, the overlap between ORF3a, ORF3c, and ORF3d potentially represents a rare example of all three possible reading frames of the same sequence region encoding functional proteins.[5][6]
Although ORF3a is present in Sarbecovirus, it is absent in another Betacoronavirus subgenus, Embecovirus, which includes the human coronaviruses HKU1 and OC43. It may be distantly related to ORF5 in Merbecovirus, which includes MERS-CoV. Distant homologs of ORF3a have been identified in Alphacoronavirus, which includes the human coronaviruses 229E and NL63, but not in Gammacoronavirus or Deltacoronavirus.[1]
Structure
The ORF3a protein is a transmembrane protein that contains three transmembrane domains. It has an N-terminal ectodomain and C-terminal endodomain, which is separated from the transmembrane domain by a cysteine-rich region.[3][2] It is thought to function as a dimer or tetramer, which is assembled at the plasma membrane. It may also form higher-order oligomers, with unknown functional effects.[3][2][1]
Post-translational modifications
In SARS-CoV, post-translational modification of ORF3a by O-glycosylation has been observed.[3][7] In hCoV-NL63, it is N-glycosylated.[8]
Expression and localization
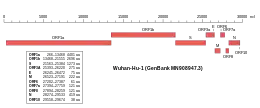 Genomic organisation of isolate Wuhan-Hu-1, the earliest sequenced sample of SARS-CoV-2, indicating the location of ORF3a | |
| NCBI genome ID | 86693 |
|---|---|
| Genome size | 29,903 bases |
| Year of completion | 2020 |
| Genome browser (UCSC) | |
Along with the genes for other accessory proteins, the ORF3a gene is located near those encoding the structural proteins, at the 3' end of the coronavirus RNA genome. ORF3a is located between the spike (S) and envelope (E) genes.[3] ORF3a is expressed from the second-largest subgenomic RNA.[2] In SARS-CoV, subcellular localization is diverse and it can be found in the cytoplasm, at the plasma membrane, and in the Golgi apparatus.[3][2] Its sequence contains protein trafficking signals that target it to the plasma membrane.[3] In hCoV-NL63, it is targeted to the ERGIC.[8]
Function
The ORF3a protein does not appear to be essential for viral replication. From studies with SARS-CoV, there is conflicting evidence on whether or not its deletion reduces replication efficiency.[3][2]
Viroporin
The ORF3a protein is thought to form a cation-permeable ion channel.[3][1][9] It is believed to function as a viroporin.[1] Along with the envelope protein, it is one of two possible viroporins in SARS-CoV-2, and one of three in SARS-CoV, which encodes the additional possible viroporin ORF8a.[1]
Viral protein interactions
The ORF3a protein in SARS-CoV has been shown to form protein-protein interactions with several structural proteins - spike protein, membrane protein, and nucleocapsid protein - as well as ORF7a, another accessory protein.[3] Through the cysteine-rich region, it may form disulfide bonds to the spike protein.[3][2] Incorporation of the ORF3b protein into virions has been observed for SARS-CoV[3][2] and hCoV-NL63,[8] indicating that it is a viral structural protein.
Host cell effects
A number of effects of ORF3a on the host cell have been described under experimental conditions. ORF3a has been associated with induction of apoptosis in studies of both SARS-CoV and SARS-CoV-2 in cell culture.[3][2][4]
Immunogenicity
The ORF3a protein is antigenic and antibodies have been observed in patients recovered from infections with SARS-CoV (which causes the disease SARS)[3][2] or with SARS-CoV-2 (which causes COVID-19).[1]
References
- 1 2 3 4 5 6 7 8 9 10 Kern, David M.; Sorum, Ben; Mali, Sonali S.; Hoel, Christopher M.; Sridharan, Savitha; Remis, Jonathan P.; Toso, Daniel B.; Kotecha, Abhay; Bautista, Diana M.; Brohawn, Stephen G. (July 2021). "Cryo-EM structure of SARS-CoV-2 ORF3a in lipid nanodiscs". Nature Structural & Molecular Biology. 28 (7): 573–582. doi:10.1038/s41594-021-00619-0. PMC 8772433. PMID 34158638. S2CID 235609553.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Liu, Ding Xiang; Fung, To Sing; Chong, Kelvin Kian-Long; Shukla, Aditi; Hilgenfeld, Rolf (September 2014). "Accessory proteins of SARS-CoV and other coronaviruses". Antiviral Research. 109: 97–109. doi:10.1016/j.antiviral.2014.06.013. PMC 7113789. PMID 24995382.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 McBride, Ruth; Fielding, Burtram (7 November 2012). "The Role of Severe Acute Respiratory Syndrome (SARS)-Coronavirus Accessory Proteins in Virus Pathogenesis". Viruses. 4 (11): 2902–2923. doi:10.3390/v4112902. PMC 3509677. PMID 23202509.
- 1 2 3 Redondo, Natalia; Zaldívar-López, Sara; Garrido, Juan J.; Montoya, Maria (7 July 2021). "SARS-CoV-2 Accessory Proteins in Viral Pathogenesis: Knowns and Unknowns". Frontiers in Immunology. 12: 708264. doi:10.3389/fimmu.2021.708264. PMC 8293742. PMID 34305949.
- ↑ Nelson, Chase W; Ardern, Zachary; Goldberg, Tony L; Meng, Chen; Kuo, Chen-Hao; Ludwig, Christina; Kolokotronis, Sergios-Orestis; Wei, Xinzhu (1 October 2020). "Dynamically evolving novel overlapping gene as a factor in the SARS-CoV-2 pandemic". eLife. 9: e59633. doi:10.7554/eLife.59633. PMC 7655111. PMID 33001029.
- ↑ Jungreis, Irwin; Nelson, Chase W.; Ardern, Zachary; Finkel, Yaara; Krogan, Nevan J.; Sato, Kei; Ziebuhr, John; Stern-Ginossar, Noam; Pavesi, Angelo; Firth, Andrew E.; Gorbalenya, Alexander E.; Kellis, Manolis (June 2021). "Conflicting and ambiguous names of overlapping ORFs in the SARS-CoV-2 genome: A homology-based resolution". Virology. 558: 145–151. doi:10.1016/j.virol.2021.02.013. PMC 7967279. PMID 33774510.
- ↑ Oostra, M.; de Haan, C. A. M.; de Groot, R. J.; Rottier, P. J. M. (March 2006). "Glycosylation of the Severe Acute Respiratory Syndrome Coronavirus Triple-Spanning Membrane Proteins 3a and M". Journal of Virology. 80 (5): 2326–2336. doi:10.1128/JVI.80.5.2326-2336.2006. PMC 1395384. PMID 16474139.
- 1 2 3 Müller, Marcel A; van der Hoek, Lia; Voss, Daniel; Bader, Oliver; Lehmann, Dörte; Schulz, Axel R; Kallies, Stephan; Suliman, Tasnim; Fielding, Burtram C; Drosten, Christian; Niedrig, Matthias (December 2010). "Human Coronavirus NL63 Open Reading Frame 3 encodes a virion-incorporated N-glycosylated membrane protein". Virology Journal. 7 (1): 6. doi:10.1186/1743-422X-7-6. PMC 2819038. PMID 20078868.
- ↑ Lu, Wei; Zheng, Bo-Jian; Xu, Ke; Schwarz, Wolfgang; Du, Lanying; Wong, Charlotte K. L.; Chen, Jiadong; Duan, Shuming; Deubel, Vincent; Sun, Bing (15 August 2006). "Severe acute respiratory syndrome-associated coronavirus 3a protein forms an ion channel and modulates virus release". Proceedings of the National Academy of Sciences. 103 (33): 12540–12545. Bibcode:2006PNAS..10312540L. doi:10.1073/pnas.0605402103. PMC 1567914. PMID 16894145.
