| Part of a series on the |
| COVID-19 pandemic |
|---|
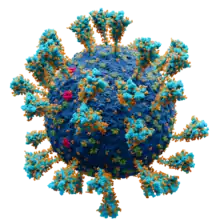 Scientifically accurate atomic model of the external structure of SARS-CoV-2. Each "ball" is an atom. |
|
|
|
The COVID-19 pandemic has had far-reaching consequences beyond the spread of the disease itself and efforts to quarantine it, including political, cultural, and social implications.
Political impacts
A number of provincial-level administrators of the Chinese Communist Party (CCP) were dismissed over their handling of the quarantine efforts in Central China, a sign of discontent with the political establishment's response to the outbreak in those regions. Some experts believe this is likely in a move to protect Communist Party general secretary Xi Jinping from people's anger over the coronavirus pandemic.[1] Some commentators have suggested that outcry over the disease could be a rare protest against the CCP.[2] Additionally, protests in the special administrative region of Hong Kong have strengthened due to fears of immigration from mainland China.[3] Taiwan has also voiced concern over being included in any travel ban involving the People's Republic of China (PRC) due to the "one-China policy" and its disputed political status.[4] Further afield, the treasurer of Australia was unable to keep a pledge to maintain a fiscal surplus due to the effect of the coronavirus on the economy.[5] A number of countries have been using the outbreak to show their support to China, such as when Prime Minister Hun Sen of Cambodia made a special visit to China with an aim to showcase Cambodia's support to China in fighting the outbreak of the epidemic.[6]
The United States president Donald Trump was criticised for his response to the pandemic.[7][8][9] He was accused of making several misleading or false claims, of failing to provide adequate information, and of downplaying the pandemic's significance.[10] Trump was also criticised for having closed down the global health security unit of the United States National Security Council, which was founded to prepare the government for potential pandemics.[11] Research suggests that the pandemic was a contributing factor to his failure to win reelection in the 2020 United States presidential election.[12]
The Government of the Islamic Republic of Iran has been heavily affected by the virus, with at least two dozen members (approximately 10%) of the Iranian legislature being infected, as well as at least 15 other current or former top government officials, including the vice-president.[13][14] Advisers to Ali Khamenei and Mohammad Javad Zarif have died from the disease.[15] The spread of the virus has raised questions about the future survival of the regime.[16]
Sovereignty
M. Nicolas Firzli, director of the World Pensions Council (WPC) and advisory-board member at the World Bank Global Infrastructure Facility (GIF), refers to the pandemic as "the Greater Financial Crisis", that will "bring to the surface pent-up financial and geopolitical dysfunctions ... [many] national economies will suffer as a result, and their political sovereignty itself may be severely eroded".[17]
Civil rights and democracy
In April 2020, UN High Commissioner for Human Rights Michelle Bachelet warned that using states of emergency during the pandemic "should not be a weapon governments can wield to quash dissent, control the population, and even perpetuate their time in power".[18][19] According to the OHCHR, around 80 countries already declared some form of state of emergency, with the most severe being among Nigeria, Kenya, South Africa, the Philippines, Iran, Jordan, Morocco, Sri Lanka, Cambodia, Uzbekistan, Peru, Honduras, El Salvador, the Dominican Republic, Uzbekistan, and Hungary.[19]
Iran, Jordan, Morocco, Oman, and Yemen banned or suspended the printing and distribution of newspapers.[20][21] On 30 March 2020, the parliament of Hungary granted Prime Minister Viktor Orbán the power to rule by decree for an indefinite period.[22]
Conflicts
The pandemic appears to have worsened conflict dynamics;[23] it has also led to a United Nations Security Council resolution demanding a global ceasefire. On March 23, 2020, United Nations Secretary-General António Guterres issued an appeal for a global ceasefire as part of the United Nations' response to the pandemic.[24][25] On 24 June 2020, 170 UN Member States and Observers signed a non-binding statement in support of the appeal,[26] rising to 172 on 25 June 2020. On 1 July 2020, the UN Security Council passed resolution S/RES/2532 (2020), demanding a "a general and immediate cessation of hostilities in all situations on its agenda," expressing support for "the efforts undertaken by the Secretary-General and his Special Representatives and Special Envoys in that respect," calling for "all parties to armed conflicts to engage immediately in a durable humanitarian pause" of at least 90 consecutive days, and calling for greater international cooperation to address the pandemic.[27]
Educational impact

The pandemic has affected educational systems worldwide, leading to the widespread closures of schools and universities.[28] According to data released by UNESCO on 25 March, school and university closures due to COVID-19 were implemented nationwide in 165 countries. Including localized closures, this affects over 1.5 billion students worldwide, accounting for 87% of enrolled learners.[29][30] Those higher education universities have also impacted their students by deciding not to stop classes but rather migrate everything to virtual. Of 195 students interview surveyed at a large university, their findings show that there is an increased concern in mental health of these students.[31] During the COVID-19 pandemic, many people who were not connected to the internet lost access to health care and education. Production in all industries was seriously harmed.[32][33][34][35]
COVID-19 and inequality
Low income individuals are more likely to contract COVID-19 and to die from it.[36] In both New York City and Barcelona, low income neighborhoods are disproportionately hit by COVID-19 cases. Hypotheses for why this is the case include that poorer families are more likely to live in crowded housing and work in the low skill jobs, such as supermarkets and elder care, which are deemed essential during the crisis.[37][38] In the United States, millions of low-income people may lack access to health care due to being uninsured or underinsured.[39] Millions of Americans lost their health insurance after losing their jobs.[40][41][42] Many low income workers in service jobs have become unemployed.[43]
Many people began teleworking during the pandemic, however teleworking has only been suitable for a tiny group of workers. Highly educated workers, usually in white-collar professions have been able to telework more than other working environments. For those still commuting to work despite the pandemic or other factors, transport remains vital.[44][45]
Religious impact

The pandemic has impacted religion in various ways, including the cancellation of the worship services of various faiths, the closure of Sunday Schools, as well as the cancellation of pilgrimages surrounding observances and festivals.[46] Many churches, synagogues, mosques, and temples have offered worship through livestream amidst the pandemic.[47] Relief wings of religious organisations have dispatched medical supplies and other aid to affected areas.[48] Adherents of many religions have gathered together to pray for an end to the pandemic, for those affected by it, as well as for the deity they believe in to give physicians and scientists the wisdom to combat the disease;[49][50][51] in the United States, Trump designated 15 March 2020 as a National Day of Prayer for "God’s healing hand to be placed on the people of our Nation".[52][53]
Healthcare and COVID-19
One of the social impacts of COVID-19 is its influence on healthcare. Two main changes in healthcare include the providers’ experience of patient care and delivery of care. With the start of COVID-19 pandemic, healthcare workers struggled to keep up with an increase in demands, a reduced capacity, increased stress and workload, and to lack of protective equipment.[54]
COVID-19 changed the perception of patient care for providers. Research about patient care during COVID-19 suggested that nurses, for example, felt more confident in their skills and role in the healthcare team. Nurses viewed their profession as essential and felt increased pride in their services, as well as, patients and other healthcare workers gained a better perspective of the nursing profession. The close contact and extensive care nurses provided during the pandemic allowed them to appreciate the nursing profession. Moreover, the research indicates that nurses achieved professional growth, and uncovered a greater need to provide counseling services for COVID-19 patients to help cope with their illness.[55] Additional research suggested a different progression to nurses’ caregiving during COVID-19. Initially, nurses experienced negative emotions associated with patient care such as increased fatigue and stressful emotions. Many nurses found self-coping styles such as teamwork and altruism to combat their fatigue. As the pandemic progressed, nurses developed a sense of gratefulness and self-reflection as opposed to the negative emotions during the initial stages of the pandemic.[56]
Healthcare delivery is another aspect of healthcare that changed during the pandemic. Most healthcare providers transitioned to providing virtual or telemedicine visits in place of traditional office visits. One study found that psychiatrists faced some barriers using telemedicine such as lack of non-verbal clues, access to internet issues, and environmental distraction. However, the overall transition to telemedicine was positive and successful, even though many patients and providers still prefer in-person interaction.[57]
For healthcare providers, there is a shared feeling of responsibility, added challenges from working with COVID-19 patients, and finding ways to be resilient. As the research finds, COVID-19 placed healthcare providers in a new environment and with unexpected challenges. Providers experienced fears of helplessness, coupled with the obligation to know answers for their patients. Other common fears included becoming infected and spreading the disease to others. To mitigate these fears, the study suggested providing extensive and regular training to healthcare professionals.[54]
Post-quarantine transmission risks
A current debate going on amongst the community involves the transmission risks post-quarantine. When COVID-19 reached the United States, the original required quarantine was 14 days of length, and later was shortened to 10 days, then 7 days, and eventually even 5 days in some places. Researchers have conducted studies using a variety of methods to analyze the statistical data behind the transmission risks. A group of researchers performed an experiment at numerous college universities, testing to examine what the post quarantine transmission risk was. From Harvard University, Duke University, Boston University, and Northeastern University, the post quarantine transmission risk after 7 days, was 13%.[58] However, the difficulty with this is that some individuals may remain communicable as short as 4 days or as long as 14 days. Another leading factor to the post quarantine transmission risks that researchers discovered, was that the different variants of covid, had different levels of contractibility.[59] After comparing the transmission risks from individuals with different strains, the Omicron strain was found to be the most communicable on day 5, but begins to balance out with the other strains in days 5-10. [59] Having differing rates of infectivity for each variant can play a role in the amount of time an individual should quarantine. This is one of the many factors affecting the post quarantine transmission risks, and more research should be done before coming to a set conclusive quarantine time.
Psychological impact
On 18 March 2020, the World Health Organization issued a report related to mental health and psychosocial issues by addressing instructions and some social considerations during the COVID-19 outbreak.[60]
Due to doubts if pets or other livestock may pass on coronavirus to humans,[61] many people were reluctant to keep their pets fearing transmission, for instance in the Arab World, celebrities were urging people to keep and protect their pets.[62] Meanwhile, people in the United Kingdom tended to acquire more pets during the coronavirus lockdown.[63]
Suicide
The coronavirus pandemic has been followed by a concern for a potential spike in suicides, exacerbated by social isolation due to quarantine and social-distancing guidelines, fear, and unemployment and financial factors.[64][65]
Risk perception
Chaos and the negative effects of the COVID-19 pandemic may have made a catastrophic future seem less remote and action to prevent it more necessary. However, it may also have the opposite effect by having minds focus on the more immediate threat of the pandemic rather than the climate crisis or the prevention of other disasters.[66]
Coronaphobia
Researchers have identified coronaphobia as a byproduct of the pandemic, where individuals have an excessive fear of contracting the virus that causes "marked impairment in daily life functioning".[67][68]
Socialization
Crowd anxiety and apprehension to pre-pandemic behavior were normalized due to the virus and subsequent lockdowns around the world. Additionally, social upheaval and other stressors have resulted in hesitancy to be comfortable sharing the same physical space with strangers.[69] In February 2021, Saturday Night Live poked fun at "post-COVID dating" after a year of isolation imagining the "weird quirks and behaviors we've picked up".[70]
Personal gatherings

The impact on personal gatherings has been strong as medical experts have advised, and local authorities often mandated stay-at-home orders to prevents gatherings of any size, not just the larger events that were initially restricted. Such gatherings may be replaced by teleconferencing, or in some cases with unconventional attempts to maintain social distancing with activities such as a balcony sing-along for a concert,[71] or a "birthday parade" for a birthday party.[72] Replacements for gatherings have been seen as significant to mental health during the crisis.[73] Social isolation among alcohol users has also adopted a trend towards Kalsarikänni or "pantsdrunking", a Finnish antisocial drinking culture.[74][75][76][77]
Domestic violence
Many countries have reported an increase in domestic violence and intimate partner violence attributed to lockdowns amid the COVID-19 pandemic.[78] Financial insecurity, stress, and uncertainty have led to increased aggression at home, with abusers able to control large amounts of their victims' daily life.[79] United Nations Secretary-General António Guterres has called for a domestic violence "ceasefire".[80]
Elderly care
Older people are particularly affected by COVID-19. They need special attention during the COVID-19 crisis, and their voices, opinions and concerns are important in formulating responses.[81]
Global data are extremely uncertain at present, nonetheless, the heightened risks of COVID-19 for older persons are evident in all national data. The scale of testing and nature of reporting vary between governments and hence there is risk of misinformation by generalizing from the experience and reports of a given country.[81]
While the number of older persons is relatively and absolutely smaller in developing countries, particularly in Africa, this coincides with other serious structural risks. Countries with the fewest older persons (such as many of the least developed countries), have the fewest health resources, limited experience caring for older patients (including few geriatric specialists), less institutional care for older persons, and far fewer public or NGO support structures for outreach, screening and community-based care of older persons.[81]
Older persons living in long-term care facilities, such as nursing homes and rehabilitation centers, are particularly vulnerable to infection and adverse outcomes from COVID-19. Older persons who live alone may face barriers to obtaining accurate information, food, medication, and other essential supplies during quarantine conditions and community outreach is required. Older persons, especially in isolation, those with cognitive decline, and those who are highly care-dependent, need a continuum of practical and emotional support through informal networks (families), health workers, caregivers, and volunteers.[81]
People with disabilities
People with disabilities are at greater risk for contracting and dying from COVID-19. This is especially true for individuals with intellectual and developmental disabilities.[82] Data from the United States indicate that people with intellectual and developmental disabilities are four times more likely to contract COVID and twice as likely to die from the disease;[83] this is likely due to the fact that people with disabilities are overrepresented in care facilities where COVID is known to spread more easily. People with disabilities are also more likely to have co-morbidities that put them at higher risk for developing COVID-related complications and may have a more difficult time socially distancing due to their support needs.[84]
People with disabilities are more likely to experience isolation and other forms of mental distress as a result of the pandemic.[85] Women and children with disabilities are more likely to experience domestic abuse during pandemics.[86]
School closures have presented children with disabilities with a host of challenges.[87][88] Many children with disabilities have seen disruptions to critical physical and occupational therapies. Many of the assistive technologies people with disabilities use are not compatible with the platforms schools are using for remote learning.[89] A large number of children with disabilities also live in poverty and may not have access to the internet and technology required for remote learning. These children may also experience a variety of social and psychological issues as the result of school closures, including food insecurity, anxiety, as well as delays in their development.[90]
See also
- Shortages related to the COVID-19 pandemic
- Xenophobia and racism related to the COVID-19 pandemic
- Distance learning
- Social impact of the COVID-19 pandemic in the Republic of Ireland
- Social impact of the COVID-19 pandemic in the United Kingdom
- Social impact of the COVID-19 pandemic in the United States
Further reading
- Durugu, S. R., Tanzeem, H., Menghani, D., Imran, Z., & Krishnan, P. (n.d.). A review of quarantine period in relation to incubation period of SARS-COV-2. ThinkIR: The University of Louisville's Institutional Repository. Retrieved September 5, 2022, from https://ir.library.louisville.edu/jri/vol4/iss1/60/
- Gowda, G., Holla, R., Ramraj, B., & Gudegowda, K. S. (2020). Contact Tracing and Quarantine for COVID-19: Challenges in community surveillance. Indian Journal of Community Health, 32, 306–308. https://doi.org/10.47203/ijch.2020.v32i02supp.025
- Hayden, M. E., Rozycki, D., Tanabe, K. O., Pattie, M., Casteen, L., Davis, S., & Holstege, C. P. (2021). COVID-19 Isolation and Quarantine Experience for Residential Students at a Large Four-Year Public University. American Journal of Public Health, 111(10), 1772–1775. https://doi.org/10.2105/ajph.2021.306424
- Zawbaa, H., Osama, H., El-Gendy, A., Saeed, H., Harb, H., Madney, Y., Abdelrahman, M., Mohsen, M., Ali, A., Nicola, M., & Ibrahim, I. Effect of mutation and vaccination on spread, severity, and mortality of COVID-19 disease. Journal of Medical Virology. (n.d.). https://onlinelibrary.wiley.com/doi/10.1002/jmv.27293
References
- ↑ Bostock B (13 February 2020). "China sacked a brace of top officials in Hubei province, likely in a move to protect Xi Jinping from people's anger over the coronavirus pandemic". Business Insider. Archived from the original on 18 February 2020. Retrieved 26 February 2020.
- ↑ Yu S (9 February 2020). "Coronavirus death toll tops Sars as public backlash grows". Financial Times. Archived from the original on 26 February 2020. Retrieved 26 February 2020.
- ↑ "Hong Kong protesters torch planned Wuhan virus quarantine building". CNA. Archived from the original on 6 February 2020. Retrieved 26 February 2020.
- ↑ "Taiwan hits out at China virus travel bans". medicalxpress.com. Archived from the original on 26 February 2020. Retrieved 26 February 2020.
- ↑ Vercoe P (February 2020). "Australia Walks Back Surplus Promise on Deadly Virus, Wildfires". Bloomberg.com. Bloomberg L.P. Archived from the original on 2 February 2020. Retrieved 14 March 2020.
- ↑ Tiezzi S (6 February 2020). "China and Cambodia: Love in the Time of Coronavirus". Archived from the original on 6 February 2020. Retrieved 10 February 2020.
- ↑ Smith D (14 March 2020). "'I don't take responsibility': Trump shakes hands and spreads blame over coronavirus". The Guardian.
- ↑ "Fact Check Friday: Trump's coronavirus response plagued with misstatements". ABC News. Archived from the original on 14 March 2020. Retrieved 15 March 2020.
- ↑ Collinson S. "Trump address sparks chaos as coronavirus crisis deepens". CNN. Archived from the original on 14 March 2020. Retrieved 15 March 2020.
- ↑ Burns K (13 March 2020). "Trump's 7 worst statements on the coronavirus pandemic". Vox. Archived from the original on 14 March 2020. Retrieved 15 March 2020.
- ↑ "Trump struggles to explain why he disbanded his global health team". MSNBC.com. 9 March 2020. Archived from the original on 15 March 2020. Retrieved 15 March 2020.
- ↑ Brodeur A, Baccini L, Weymouth S (7 December 2020). "How COVID-19 led to Donald Trump's defeat". The Conversation. Retrieved 23 December 2020.
- ↑ Cunningham E, Bennett D. "Coronavirus pummels Iran leadership as data show spread is far worse than reported". Washington Post. Archived from the original on 14 March 2020. Retrieved 15 March 2020.
- ↑ "Iran Says 10 Percent of Iranian Lawmakers Infected With Coronavirus". National Review. 3 March 2020. Archived from the original on 13 March 2020. Retrieved 15 March 2020.
- ↑ "Iran: 124 dead from virus including FM's adviser, could use force to stop travel". www.timesofisrael.com. 6 March 2020. Archived from the original on 18 March 2020. Retrieved 15 March 2020.
- ↑ "Will Iran's Regime Survive Coronavirus?". National Review. 12 March 2020. Archived from the original on 14 March 2020. Retrieved 15 March 2020.
- ↑ ""ECR Risk Experts Contemplate another Financial Crisis", Euromoney, March 20 2020 - Jeremy Weltman". Archived from the original on 5 July 2020. Retrieved 27 March 2020.
- ↑ "COVID-19: Exceptional measures should not be cover for human rights abuses and violations – Bachelet". OHCHR. 27 April 2020. Retrieved 18 June 2022.
- 1 2 "UN raises alarm about police brutality in COVID-19 lockdowns". Al Jazeera. 28 April 2020. Retrieved 18 June 2022.
- ↑ "Iran bans printing of all newspapers, citing spread of coronavirus". Committee to Protect Journalists. 31 March 2020. Retrieved 12 October 2021.
- ↑ "Jordan, Oman, Morocco, and Yemen suspend newspaper production, citing COVID-19 fears". Committee to Protect Journalists. 25 March 2020. Retrieved 12 October 2021.
- ↑ "Hungary's Viktor Orbán wins vote to rule by decree". POLITICO. 30 March 2020. Retrieved 12 October 2021.
- ↑ Mustasilta K (2020). "FROM BAD TO WORSE?: The impact(s) of Covid-19 on conflict dynamics". Conflict Series. European Union Institute for Security Studies (EUISS). Retrieved 1 August 2020.
- ↑ "Transcript of the Secretary-General's virtual press encounter on the appeal for global ceasefire". United Nations Secretary-General. 23 March 2020. Retrieved 1 August 2020.
- ↑ "COVID-19: UN chief calls for global ceasefire to focus on 'the true fight of our lives'". UN News. 23 March 2020. Retrieved 1 August 2020.
- ↑ "170 signatories endorse UN ceasefire appeal during COVID crisis". UN News. 24 June 2020. Retrieved 1 August 2020.
- ↑ "S/RES/2532(2020) - E - S/RES/2532(2020)". undocs.org. Retrieved 1 August 2020.
- ↑ McVeigh K (25 January 2022). "UN data reveals 'nearly insurmountable' scale of lost schooling due to Covid". The Guardian. Retrieved 26 January 2022.
- ↑ "COVID-19 Educational Disruption and Response". UNESCO. 4 March 2020. Retrieved 29 March 2020.
- ↑ Aristovnik A, Keržič D, Ravšelj D, Tomaževič N, Umek L (October 2020). "Impacts of the COVID-19 Pandemic on Life of Higher Education Students: A Global Perspective". Sustainability. 12 (20): 8438. doi:10.3390/su12208438.
- ↑ Son C, Hegde S, Smith A, Wang X, Sasangohar F (3 September 2020). "Effects of COVID-19 on College Students' Mental Health in the United States: Interview Survey Study". Journal of Medical Internet Research. 22 (9): e21279. doi:10.2196/21279. ISSN 1439-4456. PMC 7473764. PMID 32805704.
- ↑ "Digital infrastructure help Africa build resilient societies". European Investment Bank. Retrieved 1 September 2022.
- ↑ "COVID-19 and Africa: Socio-economic implications and policy responses". OECD. Retrieved 1 September 2022.
- ↑ "Africa and Europe: In the face of common opportunities and challenges, let's build common responses | EEAS Website". www.eeas.europa.eu. Retrieved 1 September 2022.
- ↑ "COVID-19". World Bank. Retrieved 1 September 2022.
- ↑ Fisher M, Bubola E (15 March 2020). "As Coronavirus Deepens Inequality, Inequality Worsens Its Spread". The New York Times. Retrieved 2 April 2020.
- ↑ Buchanan L, Patel JK, Rosenthal BM, Singhvi A (1 April 2020). "A Month of Coronavirus in New York City: See the Hardest-Hit Areas". The New York Times. Retrieved 2 April 2020.
- ↑ Burgen S, Jones S (1 April 2020). "Poor and vulnerable hardest hit by pandemic in Spain". The Guardian. Retrieved 1 April 2020.
- ↑ "Coronavirus May Disproportionately Hurt the Poor—And That's Bad for Everyone". Time. Retrieved 2 April 2020.
- ↑ "Coronavirus: 5.4m Americans lost health insurance during pandemic, report says". The Independent. 15 July 2020.
- ↑ "27 million Americans could lose health insurance as Congress proposes industry 'bailout'". The Independent. 13 May 2020.
- ↑ "Up to 43m Americans could lose health insurance amid pandemic, report says". The Guardian. 20 May 2020.
- ↑ Thompson D (20 March 2020). "The Coronavirus Will Be a Catastrophe for the Poor". The Atlantic. Retrieved 2 April 2020.
- ↑ "Urban mobility gets a rethink after COVID-19". European Investment Bank. Retrieved 1 September 2022.
- ↑ "COVID-19 and the shift to remote work" (PDF).
- ↑ Burke D (14 March 2020). "What churches, mosques and temples are doing to fight the spread of coronavirus". CNN. Archived from the original on 14 March 2020. Retrieved 16 March 2020.
- ↑ Parke C (13 March 2020). "Churches cancel Sunday service, move online amid coronavirus pandemic". Fox News. Archived from the original on 15 March 2020. Retrieved 16 March 2020.
- ↑ "Coronavirus Disease 2019 (COVID-19)". Evangelical Lutheran Church in America. 2019. Archived from the original on 18 March 2020. Retrieved 17 March 2020.
- ↑ Sheva A (15 February 2020). "Thousands to pray at Western Wall for end to COVID-19 epidemic". Israel National News. Archived from the original on 18 March 2020. Retrieved 17 March 2020.
- ↑ Solovy A (27 February 2020). "Coronavirus: A Prayer for Medical Scientists". Union for Reform Judaism. Archived from the original on 18 March 2020. Retrieved 17 March 2020.
- ↑ Trump D (14 March 2020). "Proclamation on the National Day of Prayer for all Americans Affected by the Coronavirus Pandemic and for our National Response Efforts". whitehouse.gov. Archived from the original on 20 January 2021. Retrieved 17 March 2020 – via National Archives.
- ↑ Casiano L (13 March 2020). "Trump declares Sunday a National Day of Prayer amid coronavirus crisis". Fox News. Archived from the original on 18 March 2020. Retrieved 17 March 2020.
- ↑ Parke C (16 March 2020). "Trump, millions go to church online on National Day of Prayer amid coronavirus". Fox News. Archived from the original on 17 March 2020. Retrieved 17 March 2020.
- 1 2 Liu Q, Luo D, Haase JE, Guo Q, Wang XQ, Liu S, Xia L, Liu Z, Yang J, Yang BX (June 2020). "The experiences of health-care providers during the COVID-19 crisis in China: a qualitative study". The Lancet Global Health. 8 (6): e790–e798. doi:10.1016/s2214-109x(20)30204-7. ISSN 2214-109X. PMC 7190296. PMID 32573443.
- ↑ Galehdar N, Toulabi T, Kamran A, Heydari H (January 2021). "Exploring nurses' perception of taking care of patients with coronavirus disease (COVID-19): A qualitative study". Nursing Open. 8 (1): 171–179. doi:10.1002/nop2.616. ISSN 2054-1058. PMC 7729793. PMID 33318825.
- ↑ Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, Wang H, Wang C, Wang Z, You Y, Liu S (June 2020). "A qualitative study on the psychological experience of caregivers of COVID-19 patients". American Journal of Infection Control. 48 (6): 592–598. doi:10.1016/j.ajic.2020.03.018. ISSN 0196-6553. PMC 7141468. PMID 32334904.
- ↑ Uscher-Pines L, Sousa J, Raja P, Mehrotra A, Barnett ML, Huskamp HA (1 November 2020). "Suddenly Becoming a "Virtual Doctor": Experiences of Psychiatrists Transitioning to Telemedicine During the COVID-19 Pandemic". Psychiatric Services. 71 (11): 1143–1150. doi:10.1176/appi.ps.202000250. ISSN 1075-2730. PMC 7606640. PMID 32933411.
- ↑ Liu AB, Davidi D, Landsberg HE, Francesconi M, Platt JT, Nguyen GT, Yune S, Deckard A, Puglin J, Haase SB, Hamer DH, Springer M (25 February 2022). "Association of COVID-19 Quarantine Duration and Postquarantine Transmission Risk in 4 University Cohorts". JAMA Network Open. 5 (2): e220088. doi:10.1001/jamanetworkopen.2022.0088. ISSN 2574-3805. PMC 8881770. PMID 35212750.
- 1 2 Wells C, Pandey A, Gokcebel S, Krieger G, Donoghue H, Singer B, Moghadas S, Galvani A, Townsend J (27 July 2022). "Quarantine and serial testing for variants of SARS-COV-2 with benefits of vaccination and boosting on consequent control of COVID-19". PNAS Nexus. 1 (3): pgac100. doi:10.1093/pnasnexus/pgac100. PMC 9335027. PMID 35909795. Retrieved 26 September 2022.
- ↑ "Mental health and psychosocial considerations during the COVID-19 outbreak" (PDF). World Health Organization. 18 March 2020.
- ↑ "Coronavirus Disease 2019 (COVID-19): If You Have Animals". cdc.gov. 11 February 2020.
- ↑ فنانون عرب في رسالة لمتابعيهم: الحيوانات الأليفة لا تنقل فيروس كورونا. arabic.cnn.com (in Arabic). 31 March 2020.
- ↑ "Households 'buy 3.2 million pets in lockdown'". BBC News. 12 March 2021. Retrieved 6 August 2021.
- ↑ Gunnell, David, et al. (21 April 2020). "Suicide risk and prevention during the COVID-19 pandemic". The Lancet. 7 (6): 468–471. doi:10.1016/S2215-0366(20)30171-1. PMC 7173821. PMID 32330430.
- ↑ Baker, Noel (22 April 2020). "Warning Covid-19 could lead to spike in suicide rates". Irish Examiner. Retrieved 27 April 2020.
- ↑ "The Guardian view on Brazil and the Amazon: don't look away | Editorial". The Guardian. 5 June 2020. Retrieved 9 June 2020.
- ↑ Arora A, Jha AK, Alat P, Das SS (December 2020). "Understanding coronaphobia". Asian Journal of Psychiatry. 54: 102384. doi:10.1016/j.ajp.2020.102384. PMC 7474809. PMID 33271693.
- ↑ ""Coronaphobia": How antivaxxers and pandemic minimizers pathologize fear of disease | Science-Based Medicine". sciencebasedmedicine.org. 16 May 2022. Retrieved 4 November 2022.
- ↑ Iovine A (16 March 2021). "FODA (Fear of Dating Again) is a thing now". Mashable. Retrieved 23 March 2021.
- ↑ Rosenberg A (28 February 2021). "'SNL' imagines the hilarious fails in store for all of our post-COVID date nights". Mashable. Retrieved 23 March 2021.
- ↑ Hassan J. "During quarantine, balconies worldwide set the stage for DJ sets, squats and singing". Washington Post. Retrieved 29 March 2020.
- ↑ Ryan S (26 March 2020). "How do you celebrate a kid's birthday during the stay-at-home order? Try a Coronavirus Caravan, with drive-by signs and songs and smiles". chicagotribune.com. Retrieved 29 March 2020.
- ↑ Janiak L (23 March 2020). "Bay Area neighbors sing and dance in social-distancing block party". Datebook. Retrieved 29 March 2020.
- ↑ "Kalsarikännit: Drinking at home in your undies, like Finns". The World from PRX.
- ↑ "It's time to embrace the Finnish tradition of drinking in your underwear". Matador Network.
- ↑ Brech A (11 April 2020). "The Finnish word for being drunk in underwear is perfect for now". Stylist.
- ↑ "What may happen after the coronavirus in Finland?". Reachinghot. 5 May 2020.
- ↑ Godbole T (9 April 2020). "Domestic violence rises amid coronavirus lockdowns in Asia". Deutsche Welle (DW). Retrieved 11 April 2020.
{{cite web}}: CS1 maint: overridden setting (link) - ↑ "UN chief calls for domestic violence 'ceasefire' amid 'horrifying global surge'". UN News. 5 April 2020. Retrieved 11 April 2020.
- 1 2 3 4 "Implications of COVID-19 for Older Persons: Responding to the Pandemic". UNFPA. 24 April 2020. Retrieved 5 June 2020.
- ↑ "Disability considerations during the COVID-19 outbreak". www.who.int. Retrieved 8 October 2020.
- ↑ "COVID-19 Infections And Deaths Are Higher Among Those With Intellectual Disabilities". NPR.org. Retrieved 8 October 2020.
- ↑ Policy Brief: A Disability-Inclusive Response to COVID-19 (PDF). United Nations. 2020.
- ↑ "How COVID-19 impacts people with disabilities". American Psychological Association. 6 May 2020. Retrieved 8 October 2020.
- ↑ Women with Disabilities in a Pandemic (COVID-19) (PDF). UN Women. 2020. Archived from the original (PDF) on 3 December 2020. Retrieved 8 October 2020.
- ↑ "Child disability and COVID-19". UNICEF DATA. Retrieved 8 October 2020.
- ↑ "Empowering students with disabilities during the COVID-19 crisis". UNESCO Bangkok. Retrieved 8 October 2020.
- ↑ Hill F (18 April 2020). "Special Education Goes Remote in the COVID-19 Pandemic - The Atlantic". The Atlantic. Retrieved 8 October 2020.
- ↑ Masonbrink AR, Hurley E (September 2020). "Advocating for Children During the COVID-19 School Closures". Pediatrics. 146 (3): e20201440. doi:10.1542/peds.2020-1440. PMID 32554517. S2CID 219906270.